Chronic pain, depression, and other problems researchers and clinicians are trying to solve with an under-studied class of drugs
Author |
This story would typically start with a description of someone hallucinating, experiencing the swirling, vibrant landscape of their consciousness. But surprise! They’re not doing acid at a party; they are in a sterile medical clinic receiving prescribed psychedelics.
It’s a common trope in articles about the use of psychedelics in medicine. But that’s not the story here.
In the exploding field of psychedelic research, Michigan Medicine is complicating that picture. Through research on psychedelics and chronic pain, treatment of depression with ketamine, and a rigorous academic approach to the topic, our researchers and clinicians are seeking nothing short of expanding our understanding of consciousness and improving patient care. There’s a palpable excitement among these thinkers, and some even exude confidence in a vision of better living through psychedelics. But there’s also an attempt to temper expectations and a commitment to doing the science right. And a distinct lack of peace signs and paisley prints.
Jump to:
Ketamine for depression
Psilocybin for chronic pain
Shamanic trance vs. psychedelics
History of ketamine research at U-M
Consciousness has at least two dimensions: the level, or how awake we are, and the content, or what we are aware of.
“While anesthetics have helped us study the level of consciousness, psychedelics offer the opportunity to modulate the content of consciousness,” says George Mashour, M.D., Ph.D., the Robert B. Sweet Professor of Anesthesiology and chair of the department as well as founding director of the Michigan Psychedelic Center. “You’re still awake, but now your perception is altered. The qualitative aspects of your experience are different.”
President Richard Nixon’s introduction of the Controlled Substances Act in 1970 began, effectively, a decades-long ban on government-sanctioned studies of psychedelic drugs, but scientists didn’t stop being interested in consciousness. They joined other advocates and lobbied for the return of rigorous studies of psychedelics.
In the early 2000s, psychedelic research reemerged and slowly ramped up over the next two decades. It is still difficult to get approval to do studies with controlled substances, but in recent years the work of academia has rippled out to broader public awareness. Cultural phenomena like Michael Pollan’s 2022 Netflix docuseries, “How to Change Your Mind” (based on his book of the same title) have introduced a lot of people to the possibilities of psychedelic research and have started to dim the stigma attached to these drugs. This resurgence of psychedelic research has meant being able to study the mind in novel ways.
“We are reopening this other dimension in the study of consciousness and leveraging the intellectual power at U-M to generate new insights into psychedelic neuroscience, to advance education, and, ultimately, to improve clinical care,” Mashour says.
What are psychedelics?
Mashour distinguishes between “classical” psychedelics — such as LSD (lysergic acid diethylamide) — and “non-classical” psychedelics, like ketamine. Classical psychedelics primarily act through 5-HT2 receptors, a subgroup of serotonin receptors that can affect cognition, mood, and perception. Though ketamine doesn’t directly affect 5-HT2 receptors, it does induce similar phenomena, such as altered perceptions, a sense of boundlessness, and intense emotions.
What seems common to all of these drugs is the way they alter consciousness. Mashour and a team of researchers recently published research that shows the similarities are not just in subjective experience but also in the brain mechanisms. They looked at the brain activity of people administered nitrous oxide and compared it to data collected in studies on LSD and ketamine. Although there were some differences, all of the drugs increased connectivity of a so-called “hot zone” in the back of the brain that is proposed to be important in determining the content of consciousness.
“It’s very interesting that the major places psilocybin interacts in the brain are serotonin receptors,” says Sagar Parikh, M.D., professor of psychiatry and the John F. Greden Professor of Depression and Clinical Neuroscience. He treats patients in the U-M ketamine clinic.
“It also helps debunk the idea that taking psychedelics is like having opiates and being high on cocaine or something like that,” he says. “Those [drugs] work on different receptors and are associated with intoxication. People who take psilocybin are having a trip, but the fact that the trip also highly activates receptors that are classically understood to be important in depression means that serotonin is involved.”
“This is not a hippie trippy endeavor”
Negative sentiment against psychedelic drugs still clings to the field of psychedelic study. But Mashour wants to change that perception.
“There’s a lot of baggage when you use the word psychedelic, but this is not a hippie trippy endeavor,” he says. “We are rigorous scientists, responsible physicians, and serious academics.”
They are also multidisciplinary. Faculty from across the U-M campus are collaborating with Medical School researchers at the Michigan Psychedelic Center. Some have obvious connections to medicine, such as the School of Social Work and the School of Public Health, but the center is also leveraging the creativity of collaborators in areas like the School of Music, Theatre, and Dance to accelerate scientific discovery and improve patient care.
For example, Christopher Sies, a percussionist who recently earned a DMA from U-M, investigated the effect of psychedelics on how we hear music, particularly the perception of timbre, or colors of sound. Inspired by both anecdotal accounts and empirical studies on psychedelic states, he created Sensate | Sublimate, his dissertation work for solo percussion, live electronics, and visual media that is designed to resemble, or even enhance, psychedelic experiences of music.
The U-M Herbarium is another collaborator with the Michigan Psychedelic Center.
“U-M has one of the largest herbariums in the world, with nearly two million plant specimens,” says David Sherman, Ph.D., professor of microbiology and immunology as well as the Hans W. Vahlteich Professor of Medicinal Chemistry. “We have 280,000 fungi samples that modern chemical methods have not even begun to explore. Many of them could contain interesting psychedelic compounds.”
Ketamine for depression
As schedule 1 drugs, classical psychedelics are currently only allowed to be used for research, but ketamine is available for clinical use in treatment of depression and pain management.
A collaborative clinical trial between U-M and the Mayo Clinic is testing the effectiveness of ketamine and looking for biomarkers that would indicate whether or not ketamine will be successful for an individual patient.

The researchers gave IV ketamine to patients with treatment-resistant depression. Then those patients were divided into two groups, those who responded well to the treatment and those who didn’t. The researchers are looking at differences in chemicals in the blood of these two groups to determine how ketamine works for different patients and to potentially find a biomarker that would indicate ketamine as an effective treatment.
Although the study results have not beenpublished yet, Parikh is happy to share one finding: 52% of the patients who received IV ketamine responded well. On average, the subjects had tried four to six medications for depression and had been depressed for many months. Many were suicidal and had been hospitalized at some point. For a group like this, Parikh says, the chance of a new antidepressant having a positive effect is about 15%.
“Half the sample, with just three infusions in 11 days, had total remission of severe depression,” he says. “Some of the sickest people did the best.”
This brings Parikh a lot of hope. “As someone who’s been treating depression for decades, you feel good knowing that for more than half your patients, you can say, ‘This is going to work for you.’”
“I can feel my brain rewiring itself”
Erin (not her real name) is in her late 20s now, but she was diagnosed with depression at age14. She has tried many traditional treatments, including talk therapy and medication. “I was on every SSRI, it felt like,” she says. She also tried Wellbutrin and an antipsychotic.
She had heard about the use of ketamine for treatment-resistant depression but knowing that ketamine has been used illegally as a recreational drug (aka special K), she was leery of going to clinics that seemed to approve every patient who was interested. She was confident that U-M would be a safe place to try something new.
At high enough doses, ketamine is an anestheticand has been used for surgery on humans and larger animals (which is how it got its reputation as a “horse tranquilizer”). At lower doses, it induces alterations in emotions and perceptions.
“There are concerns because ketamine has been a drug of abuse,” says Avinash Hosanagar, M.D., associate professor of psychiatry. “But doses people use for intoxication are much, much higher than ketamine infusion for depression.”
For Erin, the experience of a ketamine infusion is “definitely weird,” but it’s not a lot of fun. “I kind of feel like I’m floating, and I get double vision,” she says. She has found it helpful to listen to soothing, ambient music.
“I have PTSD-like symptoms from past trauma, and it’s allowed me to think events in a more detached way because it’s a dissociative medication,” Erin says. It has also contributed to healing conversations with her therapist and has enabled her to use coping strategies she learned over years in cognitive behavioral therapy.
“I was trained in CBT and didn’t find it very useful until I started doing ketamine. All of a sudden, I was able to have more emotional distance from my thoughts, even after the infusion, and analyze them in a way that CBT focuses on.
“I can feel my brain rewiring itself,” she says.
Having support is important
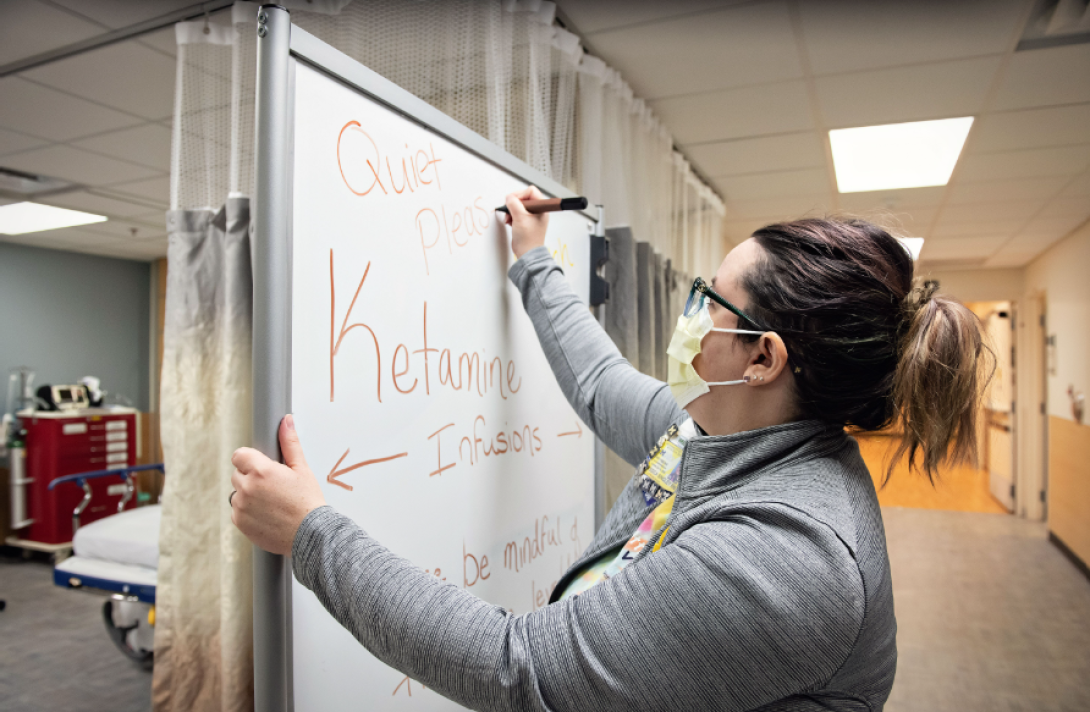
In the ketamine clinic, nurses lower the lights and put up signs encouraging everyone who comes through to be extra quiet.
“Many people don’t like the effects they experience during ketamine infusion,” says Hosanagar, who treats patients with ketamine at the VA. “Some describe being buzzed in a sense, but for many it’s not a pleasant sensation. They’re using eye shades to cut out light or listening to music to drown out external sounds, which can enhance the introspective experience to make it more enjoyable.”
Erin says a nurse stays by her side for the entire ketamine infusion. “I really, really like the nurses,” she says. “I usually have the same nurse. He’s hilarious.”
Jessica Singley, RN, a nurse in the ketamine infusion clinic says the experience varies from person to person. “Some people just get sleepy. Some people hallucinate and have seen other people in the infusion bay who aren’t there.”
“Colors are stronger,” says Elizabeth Santos-Pate, RN, who also works in the ketamine infusion clinic. “And patients might have an inability to explain their experience. You ask them, but they say, ‘I can’t find the words. It’s just weird.’”
Both nurses agree that the experience is largely calm for the patients at U-M.
Not a cure, but better
Ketamine is not a cure for depression, but Erin didn’t expect one. She told herself that if the infusions made her feel 10% better, she’d be happy.
“But I’m 20 to 30% better, which is pretty huge.”
“Qualitatively, many of my patients feel like they’re back to their old self,” says Hosanagar. “With [other] medications, though their mood improved that didn’t happen. I see that many of those who respond to treatment find joy in everyday activities. They engage with family better and are able to get back to work.”
It is important to note that ketamine treatments don’t last forever. Hosanagar says many patients stay better for weeks to months after treatment but may need more ketamine or other treatments in the future. And successful ketamine treatment doesn’t necessarily mean a patient will stop taking antidepressants. In fact, ketamine infusion at U-M is done in conjunction with other therapies.
Though ketamine is not a cure-all for depression, there is one thing it is consistently very good at treating: suicidal ideation.
“Ketamine has properties that make you stop thinking of suicide,” Parikh says. “We now have this potential of treating someone who’s been suffering a while in acute suicidal risk, and within 1.5 hours of being in the emergency room, they are no longer suicidal.”
Parikh says there are studies underway to make the case for emergency room use of ketamine.
In general, Parikh sees the main advantage of ketamine being time. “So far, we don’t have a lot of evidence that it will be wildly more successful at treating depression than traditional treatments, but it is remarkably faster.”
Hosanagar sees the same benefit: “We can make big changes in people’s lives very quickly.”
Reframing chronic pain
Kevin Boehnke, Ph.D., thinks psychedelics could help people with fibromyalgia and other conditions that cause chronic pain. But the research assistant professor of anesthesiology does not believe it will be as simple as patients taking drugs and experiencing relief. That’s why he’s leading one of the first clinical trials to see if psilocybin, in combination with talk therapy, could help people with fibromyalgia.

Boehnke’s hypothesis is that the combination of talk therapy with psilocybin will help people reframe their pain, and the myriad negative associations they have with it, so that they can engage with pain more skillfully and have support while exploring new coping strategies. This hypothesis is informed by earlier and ongoing research of psilocybin-assisted therapy for depression, post-traumatic stress disorder, and other mental health conditions.
Victoria Powell, M.D., assistant professor of geriatric and palliative medicine, has a similar theory. She’s launching a study to see if ketamine could help veterans with chronic pain and depression. Patients with these conditions can have maladaptive thought patterns, such as catastrophizing and all-or-nothing thinking.
“We know from prior research that those characteristics are commonly found in people with chronic pain conditions and depression,” she says. Although psychotherapy can be helpful for these patients, they sometimes struggle to accept the process, misinterpreting it to mean that the pain is “all in their heads.” Powell hopes that ketamine could free up this mental space to allow them to explore therapies they’ve been unwilling or unable to try before.
The journey to getting unstuck could be a quick trip
Boehnke also has a personal data point that in-forms his work. He was diagnosed with fibromyalgia when he was 21. Like many others with the condition, he had a long road to diagnosis and eventual management of his symptoms. Due to poor understanding of fibromyalgia, he got some bad advice along the way. One health care provider told him not to exercise, as doing so might exacerbate his pain. This ultimately set him back. “As long as you’re listening to your body and careful about intensity, movement is one of the most important things people can do to manage symptoms.
”A lot of people with fibromyalgia have similar experiences. At the same time, medications are often unsuccessful at treating fibromyalgia symptoms. In the subset of patients who do experience relief, the side effects of the medications can outweigh the benefits.
“Psychedelics have the potential to really help people who are stuck in these sorts of loops and behavior patterns,” Boehnke says. They can give hope to people who feel they have no treatment options. “And the sorts of insights that could show up during a psychedelic experience may help people get perspective and a different view on their life and behaviors.”
That’s where therapy comes in. A trained professional can help patients prepare for a psychedelic experience and reflect on the ways their behaviors and/or symptoms change in the aftermath.
The clinical trial Boehnke is leading involves a lengthy screening process and then therapy to help subjects prepare for their psilocybin experience. Boehnke says it’s important that patients have time to build rapport with the therapists, since “these are people with whom they’ll have a pretty intense experience.”
Subjects will then have two dosing sessions, and they’ll return after each one to process the psychedelic experience and discuss helpful themes or ideas that might have emerged. Following that, the subjects will have several therapy sessions to discuss what changes they’ve noticed in their lives and to help identify ways they can incorporate any insights they’ve had about how to manage their symptoms.
Powell’s proposed study would also include psychological support in the form of “narrative sessions.” This would be an opportunity for veterans to tell the story of their chronic pain and depression experience.
“By going through a relatively brief session with a guide trained in psychotherapy or adjacent approaches, they might be able to reframe maladaptive thoughts and get some of the benefits of psychotherapy in much less time,” she says.
Existential distress and loneliness
Powell specializes in palliative care. If her study with veterans is successful, she hopes to study the effect of psychedelics for patients in palliative care. At the end of life, existential distress, or alack of connection to others or to greater meaning in life, may complicate people’s suffering.
Although conventional mental health treatment might be helpful, Powell says, many of her patients “really don’t have the time or energy to engage in traditional psychotherapy.”
She thinks psychedelics could work much more quickly to give them relief and allow them to spend their remaining time in meaningful pursuits.
Unraveling the neurobiology behind altered consciousness
Michigan Medicine is also doing basic science research to learn more about the neurobiological effects of psychedelics. Dinesh Pal, Ph.D., associate professor of anesthesiology, and Giancarlo Vanini, M.D., assistant professor of anesthesiology, are using rodent models to investigate whether psychedelics may provide relief from chronic pain.
“We are using well established experimental models to probe ... the underlying mechanistic processes,” Vanini says.
“Due to increased recreational use, we also need to understand the effect of psychedelics on sleep,” says Pal, who is studying psilocybin and dimethyltryptamine (DMT), hallucinogens that have been used for ceremonial purposes across indigenous cultures.
Basic science research may also open the door for the wider development of medications to help patients. Because most psychedelics like psilocybin, which comes from a fungus, are natural, there’s not a lot of incentive for pharmaceutical companies to try to develop drugs for clinical use.
“You can’t patent a natural product,” says David Sherman, Ph.D., professor of microbiology and immunology as well as the Hans W. Vahlteich Professor of Medicinal Chemistry. Sherman and researchers in his lab at the U-M Life Sciences Institute are working to create new molecules, derived from the natural molecules, that optimize the performance of the psychedelic drugs.
“We can isolate a psychedelic from a plant or a fungus that we can grow in the laboratory, and then we can use our chemical tools to convert a natural product into an unnatural product. And if it works better than the natural product, we have a great intellectual property position,” Sherman says.
A psychedelic naturally occurring in the brain
Jimo Borjigin, Ph.D., did not set out to study psychedelics. Her lab in the molecular and integrative physiology department was focused on melatonin secreted by the pineal gland. While looking for teaching materials on YouTube one day, she stumbled onto videos calling the gland “the third eye” and “the seat of the soul.”
“It was a whole world I didn’t know about,” she says.
She watched DMT: The Spirit Molecule, a documentary by University of New Mexico psychiatry professor Rick Strassman, M.D. In it, Strassman said he thought endogenous DMT was made in the pineal gland of mammals, but Borjigin couldn’t find any research to back up the claim. When she contacted Strassman, he admitted that it was speculation.
Borjigin suggested that Strassman collaborate with her on a study. The results, published in 2013, proved the existence of DMT in the pineal gland of rats.
Since then, Borjigin’s lab has sought to understand whether and how DMT is synthesized in the pineal gland and what role it may play in normal brain function. They’ve shown an increase in DMT in the brains of rats experiencing cardiac arrest — a finding that lends support to the idea that DMT may be involved in near-death experiences. A 2018 UK study showed that people given DMT described similar phenomena to that of people who have had near-death experiences. Most recently, Borjigin’s lab has shown that an enzyme previously believed to be important for DMT synthesis is not involved. A pharmaceutical company funded that research, and Borjigin hopes to get funding from other sources to continue her work.
“The Michigan Psychedelic Center represents an exciting new chapter for research, education, and clinical care at Michigan Medicine,” Mashour says. “It is important not to stigmatize psychedelics, but neither should we romanticize them. Learning lessons from the past, our team is balancing enthusiasm with rigor and responsibility.”
Note: The University of Michigan strictly adheres to all animal research guidelines. In addition to those guidelines, U-M researchers are committed to principles known as “the three Rs”: reducing the number of animals used to the minimum required for the study, replacing animals with less sentient or non-animal models whenever possible, and refining all practices to provide the best animal welfare possible.