Nearly half of women in the United States have dense breasts, a factor that in some cases can raise breast cancer risk and make diagnosing the disease harder.
7:00 AM
Author |
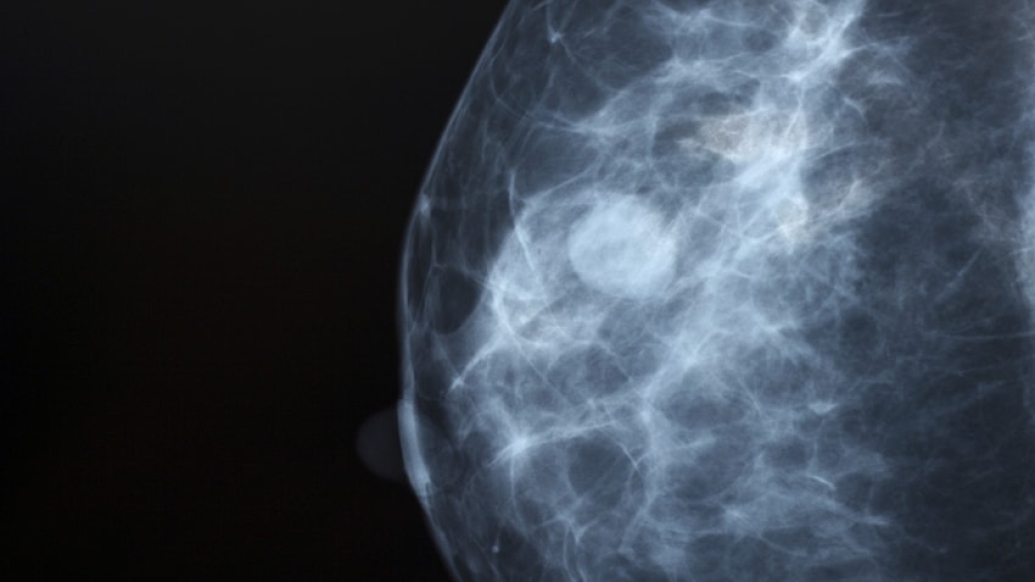
Women with high breast density have an increased risk of developing breast cancer, depending on the density level. Dense breasts, which are marked by greater amounts of fibrous and glandular tissue than fat, can make diagnosing breast cancer on mammograms tougher.
SEE ALSO: 5 Ways to Help Prevent Cancer
Considering these factors, it might seem surprising that breast density wasn't always something doctors talked about with their patients.
Which is why there's been a push to require it: In June 2015, Michigan became the 21st state to pass legislation requiring mammogram facilities to disclose a finding of dense breasts (that number has since grown to 28 states). In their results letter, women are informed if they have dense breasts, educated regarding implications and advised to discuss additional screening methods with their health care providers.
With October serving as Breast Cancer Awareness Month, Renee Pinsky, M.D., an associate professor at the University of Michigan who specializes in breast imaging, shares some information that women with dense breasts should know.
Determined only via mammogram, breast density is categorized into four levels:
a) Almost entirely fatty
b) Scattered fibroglandular densities
c) Heterogeneously dense
d) Extremely dense
Dense breasts are quite common: About 40 percent of women have heterogeneously dense breasts, and 10 percent have extremely dense breasts. Densities in levels c and d are considered dense breasts, says Pinsky.
She explains more below.
Breast density can't be diagnosed by touch: The term refers to a mammogram's appearance — not a tactile verdict attained with one's hands. How the breast feels on exam can be deceiving: "A woman's breast may feel soft but appear dense on the mammogram," Pinsky says. "A fatty or less-dense breast may have areas that feel firmer."
Cancer detection is more difficult: Fatty tissue appears gray and black on a mammogram, while cancers show up as white. Because dense breasts have high concentrations of fibrous and glandular tissues — which both look white, too — finding the cancer can be difficult. "I have used the analogy of finding a cotton ball in a snowstorm," Pinsky says. "It would be a lot easier to find that cotton ball on a black asphalt street." This phenomenon is called masking.
Dense breasts increase the risk of breast cancer: Studies have reported variable levels of increased risk. The most valuable assessment of risk, Pinsky says, is comparison with a woman with average breast density — in which case the comparative risk is 1.2 times greater for someone with heterogeneously dense breasts and 2.1 times for extremely dense breasts. Studies comparing the highest density to the lowest density have reported a four to six times increased risk of cancer.
Mammograms remain essential: No matter a woman's breast density, "mammography saves lives," says Pinsky, who says the preventive screenings should begin yearly at age 40. Breast cancer deaths have decreased by about 30 percent since the screening protocol started.
Density can change with age and lifestyle: Various events might alter breast density over time. Pregnancy, lactation, weight loss and taking postmenopausal hormones all can increase density. Menopause is a common trigger for reducing density, Pinsky says, but it isn't universal. Some women with dense breasts maintain them long into old age.
Dense breasts might require additional screening: Supplemental tests, including MRI and ultrasound, could be pursued for a closer look. That, Pinsky says, should occur after a patient and her doctor discuss risks and benefits — namely, "the risk of finding something that does not turn out to be cancer, including possible needle biopsy or surgery, versus the benefit of finding a cancer that would not have been seen on the mammogram." Every woman has her own tolerance for these issues.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





