Families occasionally struggle to decide whether to have their child’s adenoids removed. A Michigan Medicine pediatric otolaryngologist explains the procedure.
7:00 AM
Author |
The removal of a child's adenoid might prompt more questions from parents than the more familiar tonsillectomy.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
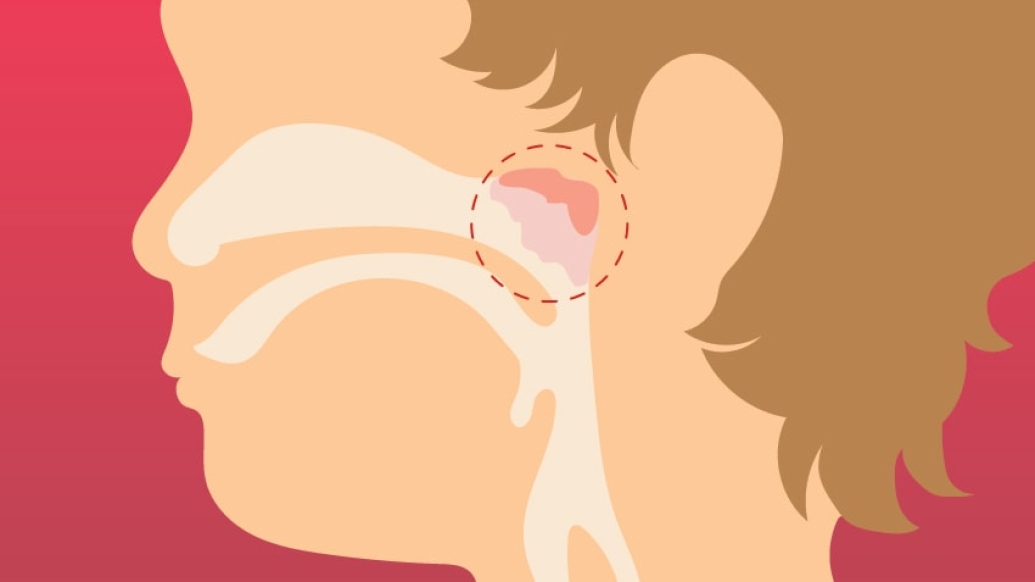
That's because the adenoid, a mass of lymphatic tissue in the back of the nose behind the soft palate, is out of sight — and conversation, too.
"Adenoids are a bit more of a mystery to parents because they're not something as commonly discussed," says Lauren Bohm, M.D., a pediatric otolaryngologist at University of Michigan C.S. Mott Children's Hospital.
Adenoids, which shrink by adolescence in most individuals, are designed to trap germs that enter through the nose. A person's tonsils maintain a similar function, catching microscopic substances that come in via the mouth.
Surgery doesn't compromise that line of defense: "Studies have shown that removal of the adenoid doesn't adversely affect a body's ability to fight off infection in the long run," Bohm says. "There's enough redundancy in the immune system."
Still, the decision to remove a child's adenoid should involve careful examination and a discussion between his or her family and their otolaryngologist.
Bohm spoke more about the basics of the surgery:
5 things to know about adenoidectomy
Why it's done
Adenoidectomy may be advised when a child has persistent nasal obstruction, chronic ear or sinus infections, snoring or sleep disturbance. Says Bohm: "If there's frequent nasal congestion and drainage, especially without other symptoms of illness, we'll usually recommend an evaluation" with an X-ray or a small camera in the nasal cavity.
Who might get it
Most enlarged adenoid cases present in early childhood, says Bohm. And a child needn't be a candidate for tonsillectomy — often spurred by frequent tonsillitis or sleep apnea (pauses in breathing at night) — to warrant adenoid removal.
SEE ALSO: Your Pediatrician vs. Urgent Care: What to Do When Your Child Is Sick
How the surgery is done
Performed as an outpatient procedure, adenoid removal takes place under general anesthetic with a breathing tube. Removal involves shaving or cauterizing the adenoid down to the base ("like cutting back a bush or shrub," Bohm notes). It's a short surgery, about 30 minutes in most cases, she says. No sutures are needed after adenoid removal.
Potential risks and complications
Anyone receiving an adenoidectomy should be "relatively healthy" at the time of the operation to ensure a quick recovery, Bohm says. But special considerations must be made for children with bleeding disorders and Down syndrome. Children with a history of a cleft palate or a neuromuscular disorder may be predisposed to speech abnormalities after the procedure.
What to expect in recovery
Compared with tonsillectomy, the healing process is often easier for adenoidectomy patients. "There's typically less pain, less risk of bleeding and a quicker return to normal activities," Bohm says. "Children may complain of some ear or throat pain, which is typically managed with Tylenol or Motrin." Still, she notes, it may take several days for symptoms to improve.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





