The body’s ability to regrow its liver facilitates an uncommon but growing form of transplantation. A surgeon talks about the procedure
7:00 AM
Author |
This article was updated on August 22, 2023.
In most cases, patients who need a new liver receive one from a deceased donor.
But some sick people find salvation from another source: living individuals.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
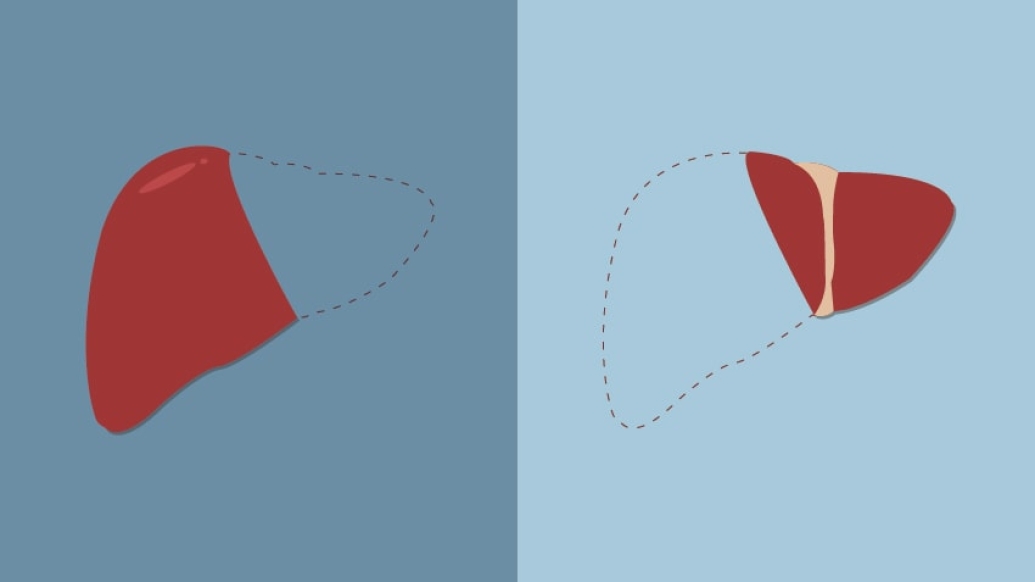
A living liver donation surgery involves removing part of a person's healthy liver — as much as 60% — and using this partial liver to replace the recipient's diseased liver. In the weeks to come, both the donor and recipient sections will grow to the size of normal livers.
The exchange, performed on adults since the late 1990s, seems like something out of science fiction.
"There aren't many other organs in the body that truly have the capacity to regrow," said Christopher Sonnenday, M.D., transplant center director and surgical director of the Adult Living Donor Liver Transplant Program at Michigan Medicine.
"It is a totally transformative operation."
It's also a crucial one.
While dialysis, for instance, can bridge kidney failure patients until a transplant becomes available, there are no alternative therapies for liver failure.
That's why liver transplants are prioritized by a recipient's level of sickness using an assessment known as a MELD score (Model for End-Stage Liver Disease).
This priority system has helped reduce deaths on the waiting list, but also requires patients to become critically ill before having the opportunity for a lifesaving transplant, Sonnenday says.
Still, demand far exceeds supply: More than 14,000 people in the United States are waiting for a new liver, according to the United Network for Organ Sharing. Livers are the second most-needed organ after kidneys.
Without a timely and suitable match, "the critically ill people are essentially dying of their disease without having a chance," said Sonnenday.
This is why a small but growing number of individuals are opting to give a part of their liver to help someone else — demand that is driving a need for more living donor liver transplant programs.
Sonnenday talks about the procedure, and what all involved parties should know:
Facts about living liver donation
Many, but not all, donors know their recipient: Because of the size and scope of the operation — plus the speed a decision to donate might require — a living liver donor typically has close ties to the recipient.
Still, both sides must undergo a range of compatibility tests.
One problematic issue: if a donor's body is much smaller than the recipient. In these cases, "the portion of their liver might not be adequate" for the sick patient's needs, Sonnenday said.
Individuals that come forward to donate to anyone on the list, known as “non-directed” donors, are evaluated as donors to children and other individuals who may face particular challenges finding an appropriate deceased donor.
Living donations save time: Living donation is intended to help a sick patient avoid the wait time for a deceased donor.
That can mean an individual receives lifesaving intervention before his or her condition (typically end-stage liver failure, liver cancer or other rare and metabolic diseases) worsens.
Noted Sonnenday: "Seeing someone they love waste away is often the motivating factor. It allows them to 'jump the line' and have the opportunity to become well."
SEE ALSO: Strength in Numbers: Why Organ Donation Matters [Infographic]
Live liver donations remain rare: Living liver donation was first attempted in children in the late 1980s.
Adult transplants initially took place a decade later, Sonnenday says. Today, they account for only about 7% of total liver transplants.
That's partially because the surgery can frighten or disqualify some donors — and there are limited surgeons and centers with robust expertise.
The latter is changing, with national and international collaborative efforts among centers to share expertise and experience.
Risks affect both parties: Studies have shown that "long-term outcomes are as good or better" for living-donor recipients, Sonnenday says.
But unique challenges remain. Because it's only part of a liver, the implantation process for the recipient is more complicated. T
here also are risks to the donor, such as bleeding and the need for blood transfusion.
The mortality rate for the donor, Sonnenday says, is approximately 1 in 600 — a rare outcome, but an important piece of information for donors to consider.
Recovery time is significant: A living donor who gives a kidney might be hospitalized for a few days and spend four to six weeks healing.
Those who offer part of their liver, however, can expect to double that length of time. "It's a bigger operation," said Sonnenday, noting that long-term data show no signs that the surgery affects a donor's life span or risk of developing liver disease.
Meanwhile, it takes about four to six weeks for both parties' livers to grow to full size.
Recipients bounce back: Whether due to the generosity of a living or deceased donor, transplant surgery is transformative.
"I see (recipients) eight or 12 weeks after their surgery and you can't even recognize them. They look like new people — muscle mass, color in their face, vigorous and energetic," said Sonnenday.
"To see that happen through the generosity of living donation is truly a miracle we are honored to witness."

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





