A patient with advanced heart failure gives birth to a healthy baby thanks to Michigan Medicine’s Cardio-Obstetrics Program.
9:44 AM
Author |

Sheila Galinis was thrilled to discover she was having a baby with the man she loved and able to give her 9-year-old son, Makaiah, a brother.
But, as she quickly learned in May 2020, this pregnancy would not be as smooth as her first. In fact, doctors urged Galinis to consider ending her pregnancy in an effort to save her life.
The 37-year-old had been diagnosed with advanced heart failure five years earlier, a condition that put her at high risk for significant complications during pregnancy.
But Galinis, also diagnosed with asthma, was determined to continue her pregnancy, despite symptoms that would only grow worse during the coming months.
"I knew it was risky, but I truly believed the stress of terminating my pregnancy would be far more detrimental to my health than going through with it," she says.
Heart failure occurs when the heart muscle can't pump enough blood to meet the body's nutrition and oxygen needs. The blood begins to back up and, as a result, the veins, tissues and lungs become congested with fluid. Symptoms often include shortness of breath, exhaustion and high blood pressure.
"The expertise I needed"
With a recommendation to consider the Michigan Medicine Cardio-Obstetrics Program, Galinis was introduced to a team of specialists that included Elizabeth Langen, M.D., Ashley Hesson, M.D., Ph.D., and Melinda Davis, M.D.
"I was told Michigan Medicine had the ability to manage my care. They could provide the expertise I needed," says the White Pigeon, Michigan, resident.
But Galinis was not out of danger.
"Sheila came to us at 22 weeks of pregnancy with a diagnosis of heart failure as well as poorly controlled asthma," says Hesson. "We sat down with her to discuss the risks based on her severe heart condition."
MORE FROM MICHIGAN: Sign up for our weekly newsletter
These risks included the potential to develop an irregular heartbeat, also known as an arrhythmia, or acute decompensated heart failure — a sudden worsening of her heart failure condition. She also was faced the possibility of a future heart assist device to support her heart, or even a heart transplant, says Hesson.
There was always fear in the back of my mind, but I didn't want to dwell on that. I have a life to live and wanted to continue to get better for my family.Sheila Galinis
Of even greater concern, Galinis faced a 20% chance of not surviving, says Langen, noting nationwide studies have revealed that more than one-quarter of maternal deaths are related to cardiovascular disease such as heart failure.
Unmasking the symptoms
"Sheila's condition was complicated because the symptoms of heart failure are also the symptoms of a normal pregnancy such as fluid retention and difficulty breathing," says Langen. "It's also difficult to distinguish heart failure symptoms from asthma."
For example, says Hesson, "When Sheila experienced an upper respiratory infection in early October, she was admitted to the hospital for several days for stabilization. She was struggling to breath at times and it was difficult to determine if that was due to worsening of her heart condition, her asthma or the infection."
After the infection cleared, Galinis' care team — including experts in maternal fetal medicine, advanced heart failure, cardiology, adult congenital cardiology, nursing, pharmacy and anesthesiology — met several times to determine the best recommendation for her mode of delivery (vaginal or cesarean), timing of delivery and any additional resources for support that would be necessary to optimize safety.
"We were very careful to weigh every possible complication," says Langen.
"The team collectively recommended that she undergo right heart catheterization to more specifically determine her heart function and estimate her risk of acute decompensation as well as the likelihood of needing invasive monitoring or cardiopulmonary support at the time of delivery," says Hesson.
"She underwent the catheterization and the numbers were somewhat reassuring. Again, we met with the team, discussed the options with Sheila, and agreed on a 32-week delivery. This timing was chosen to try to optimize neurological and respiratory outcomes for the baby without incurring any additional undue risk for Sheila."
Galinis' care also involved weekly calls from the cardio-obstetrics team and frequent visits with the team to adjust her medications, monitor her symptoms and ensure that her baby was growing well.
Shared decision-making
Equally important, says Hesson, is the Cardio-Obstetrics Program's commitment to patient communication. "We strive for a deep understanding of our patients' goals and try to support all viewpoints. We listen to women and to what their bodies are telling us to help pinpoint what's going on and to enable us to provide the best possible care."
"Our team works in partnership with our patients to decide the best course of action, including optimal timing for delivery — with a focus on what's best for the mother and baby. It's a shared decision," says Langen.
In Galinis' case, this shared decision was to try for a vaginal birth, but because the baby was breech, the team recommended a cesarean delivery.
Like Podcasts? Add the Michigan Medicine News Break on iTunes, Google Podcast or anywhere you listen to podcasts.
Focused on lifelong health
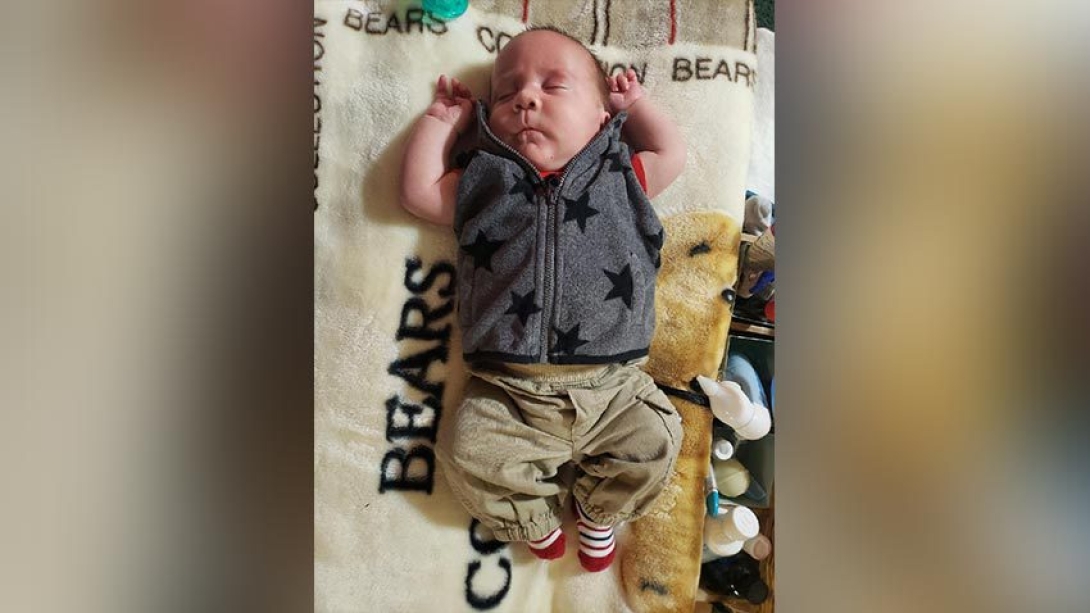
Galinis is happy to report that her baby, named Charlie, was born at 32 weeks via cesarean delivery. Weighing 5 lbs., 7 oz., he was in an incubator and monitored for a month before coming home just in time for Christmas.
The mother of two believes she made the right decision, but says, "There was always fear in the back of my mind, but I didn't want to dwell on that. I have a life to live and wanted to continue to get better for my family."
Now in the care of an advanced heart failure team, Galinis is committed to her health. It's this type of ongoing care that is critical to the patient's heart failure condition, says Hesson.
"We try to impart the importance of our patients transitioning from the care they received during pregnancy to care across their lifespan. We want to engage them to care for their lifelong health."

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





