A Michigan Medicine nurse recently studied how to reduce urinary retention issues in patients anesthetized for outpatient surgery. Now, her work has wider potential.
7:00 AM
Author |
Two years ago, Lori Dager, R.N., spotted a troublesome trend: More and more patients had to be catheterized before heading home from the outpatient surgery center where she worked.
MORE FROM THE LAB: Subscribe to our weekly newsletter
The reason: postoperative urinary retention (POUR), an inability to urinate after having anesthesia.
"I just know we were catheterizing patients, who sometimes had near a liter of urine, which is not good for the bladder," says Dager, who works in the post anesthesia care unit (PACU) at the East Ann Arbor Surgery Center.
"It's traumatic being catheterized and it extends the stay at PACU."
Urinary retention is a common complication that arises after a patient has anesthesia or surgery. The analgesic drugs often disrupt the neural circuitry that controls the nerves and muscles in the urination process. This can lead to abnormal storage of urine because patients often don't feel like they have to urinate despite having a full bladder.
Distention of the bladder stretches its muscular wall, called the detrusor muscle, and can permanently damage the bladder in as short as one to two hours.
Which is why Dager recently completed an evidence-based practice project designed to curtail instances of POUR.
Her project has since prompted a change in recovery room protocol, which is being rolled out at other PACUs in Michigan Medicine after early efforts showed a decrease in POUR cases.
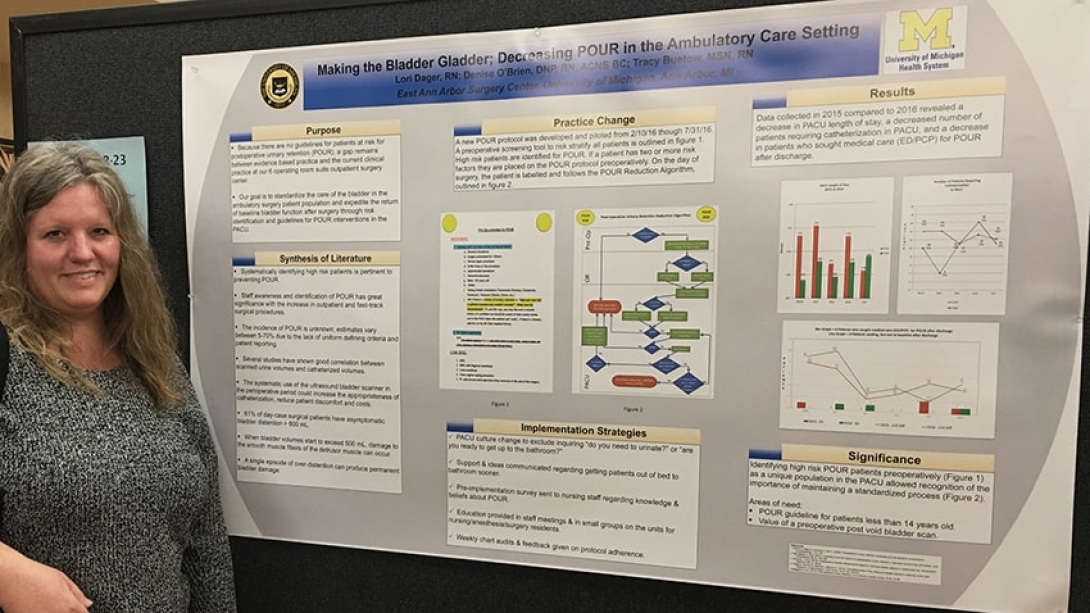
The results were shared with colleagues at the American Society of PeriAnesthesia Nurses national conference in April in Indianapolis, via a poster presentation titled "Making the Bladder Gladder; Decreasing POUR in the Ambulatory Care Setting."
"I gave it a catchy title because there are about 100 posters at the national conference and 'Bladder Gladder' helped make it stand out," Dager says. "POUR is not something all nurses are tuned in to, so raising awareness will help with the prevention aspect."
Dager says her findings will hopefully prompt more research in this area.
Her mentor, Denise O'Brien, D.N.P., R.N., will also showcase the work at the International Conference for PeriAnaesthesia Nurses in Sydney, Australia, this year.
Taking action
The prevalence of POUR is unknown. Estimates vary between 5 to 70 percent of people who received an anesthetic during surgery due to the lack of uniform defining criteria and patient reporting, Dager's literature search revealed.
SEE ALSO: Nursing Homes Cut UTIs in Half Through a Focused Effort on Catheter Care
Although catheterization can be used to empty the bladder in these circumstances, regardless of a recipient's age, the procedure carries risk. According to the Centers for Disease Control and Prevention, approximately 75 percent of UTIs acquired in the hospital are associated with a catheter.
To avoid a catheter (and any potential complications), Dager encouraged her patients to urinate, even if they said the need was absent — advice that she learned wasn't a uniform practice.
"It felt like every nurse was doing something different at the bedside," Dager says. "I couldn't help but wonder if we changed our culture or streamlined our process, maybe we could prevent problems like POUR."
Soon after that thought in 2015, Dager received a hospitalwide email from the Nursing Research and Translation Committee asking about areas of interest to improve quality care by making changes at the bedside.
Dager wrote back with interest about POUR, not realizing she was applying to be in the first cohort of the Staff Nurse Evidence-Based Practice Fellowship, a one-year honor awarded annually to six Michigan Medicine nurses. The fellowship provides the opportunity for staff nurses to take a clinical idea, explore the evidence surrounding it and, with guidance provided by institutional leaders, make a practice change to improve patient care.
Prevention has long been the mantra of Dager, a Michigan Medicine employee for nearly three decades.
"I enjoy being at a teaching hospital like the University of Michigan because we have a culture of sharing knowledge and collaboration," she says.
Setting new standards
Dager focused on standardizing care of the bladder and expediting the return of baseline bladder function by identifying risk factors preoperatively, creating an algorithm on the steps to take.
SEE ALSO: What It Takes to Protect Hospital Patients from UTIs
She also used a bladder ultrasound scanner as soon as patients arrived in the recovery room after surgery, particularly when a patient had two or more risk factors, including personal health history, certain types of surgery and current medications.
Dager knew she was onto something when she began fielding phone calls from other PACUs and urology experts when word of her POUR project spread.
Still, one of the most difficult but effective elements was changing the language that nurses used with their patients.
"We had to change our culture," Dager says. "We had to quit asking them, 'Do you need to urinate?' or 'Are you ready to get up to the bathroom?' Instead, we told them it's time to void now, and that prompt comes much earlier in their recovery phase, rather than before leaving the surgery center."
Dager piloted the project at the East Ann Arbor Surgery Center from February to July 2016.
Compared to data collected in 2015, results following her new protocol were significant: PACU length of stay dropped. It also cut the number of patients requiring catheterization and reduced the number of patients seeking care for POUR after discharge.
Based on that success, Michigan Medicine is implementing Dager's protocol in other PACUs.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





