Christina Costa’s case required multiple neuro specialists. A multidisciplinary brain tumor clinic offered her just that, in one location.
1:50 PM
Author |
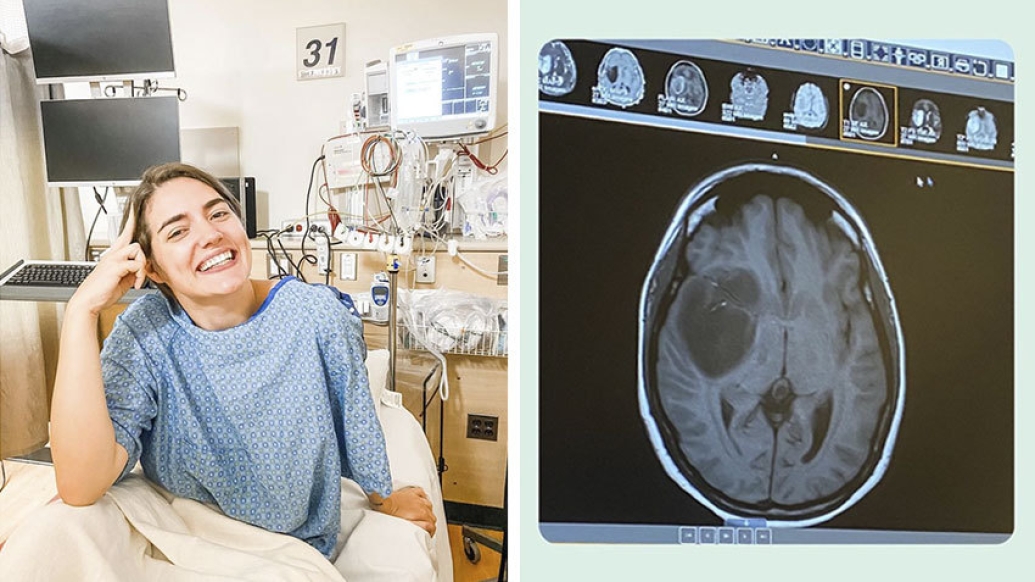
Just over a year ago, Christina Costa was focused on her third year as a University of Michigan psychology student working toward a Ph.D. But testing for what she believed were migraine headaches would temporarily take her life in a new direction.
Because Christina's father had a history of migraines, she thought hers might have a genetic origin. But when she began experiencing vision issues and, later, dizziness and numbness in her left hand and leg as well as in her face, the 27-year-old was seen by Michigan Medicine neurologist Sayyed Sohrab, M.D.
A frightening diagnosis
Sohrab ordered a routine MRI that revealed a type of brain tumor known as a glioma. This tumor often occurs near areas of the brain that control body movement, language or vision. Gliomas have different subtypes, with astrocytomas being some of the most common. They typically have boundaries that are not well defined, with small clusters of tumor cells infiltrating surrounding healthy tissue. Some of these tumors are considered malignant or cancerous, while others are considered more benight or low-grade. Low-grade gliomas are most commonly diagnosed in young patients.
In addition to the recommended treatment of surgery for both cancerous and non-cancerous tumors, patients may undergo chemotherapy and radiation.
Costa was immediately referred to Michigan Medicine neurosurgeon Wajd Al-Holou, M.D., who would team with neuro-oncologist Yoshie Umemura, M.D., and radiation-oncologist Daniel Wahl, M.D., of the Michigan Medicine Multidisciplinary Brain Tumor Clinic (M3BTC). The Clinic is uniquely designed to help patients effectively manage their care by having them meet with the neurosurgeon, neuro-oncologist and radiation-oncologist all together in one setting.
"Our goal is to work as a team to develop personalized treatment recommendations that are unique and will maximize the benefits for each patient," says Al-Holou, noting the team's extensive expertise in treating both malignant and benign tumors.
Another key differentiator is the Clinic's ability to offer patients access to state-of-the-art clinical trials.
A challenging surgery
Costa's tumor was very large and in a challenging location, says Al-Holou, who performed an awake surgery to remove as much of the tumor as possible on September 8, 2020.
"Christina's tumor was located within the insula, which is buried deep within the brain and surrounded by critical blood vessels and bordered by essential brain fibers that control important functions such as movement, sensation and vision," says Al-Holou.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
"These types of tumors lack a clear margin and frequently infiltrate eloquent areas of the brain, thus making their surgical resection challenging," he says, noting that new approaches have given his team unique expertise in treating astrocytomas, particularly those within the insula.
"Many health care systems don't have this expertise. We use a combination of state-of-the-art surgical techniques and technologies to maximize tumor resection, avoiding injury to the brain and giving our patients the best chance of returning to a normal life," says Al-Holou.
"It was important that Christina be able to drive and function normally after surgery, so we took extra time to do this complex awake surgery. In Christina's case, we knew based on our testing where her critical motor, sensory and vision fibers were and we were able to remove the tumor right up to those fibers without injuring them."
Coordinated care
Costa, who is currently undergoing chemotherapy and radiation, is happy to report that 97% of her tumor was removed.
"After surgery, we often recommend a combination of chemotherapy and radiation to decrease the chance of or delay any recurrence," say Al-Holou. "Christina was seen in our M3BTC to immediately help coordinate those consultations with our neuro-oncology partner, Dr. Umemura, and our radiation-oncology partner, Dr. Wahl," says Al-Holou.
As Costa continues her recovery and gains strength, she feels fortunate to have been one of the first patients to experience the benefits of the Michigan Medicine Multidisciplinary Brain Tumor Clinic.
Like Podcasts? Add the Michigan Medicine News Break on iTunes, Google Podcast or anywhere you listen to podcasts.
"I met with all of my doctors at one time to determine my treatment plan. It's so cool to be able to meet with all three in a single appointment," she says. "It's comforting to know they're a team and that they all work together as colleagues."
Another plus for Costa is the ability to stay connected with her surgeon.
"Because of the Clinic, I know I'll see Dr. Al-Holou as well as the other doctors," she says. "It's great to have him as part of my follow-up care because he's the person who was so involved from the start."
Costa recalls Al-Holou's patience during the initial consultation when he took extra time to answer her many questions as well as those of her parents and husband, Adriano.
Looking forward
Al-Holou says Costa's prognosis is good and is helped by her motivation and commitment to healing. "Christina is a very determined patient and is incredibly focused on using her experience to teach and help others."
For her part, Costa is eager to finish her dissertation and get back to teaching in the U-M psychology department.
As a proactive measure, she had her embryos preserved with the help of friends who raised money for the procedure. It's her hope that she and her husband will one day be able to start a family.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





