Problems with her placenta inspired physician Courtney Townsel to specialize in helping others understand the high risk pregnancy conditions that impact this vital organ.
1:03 PM
Author |
For Courtney Townsel, M.D., M.Sc., working with patients experiencing high risk pregnancy conditions involving the placenta is a lived experience.
Townsel, an obstetric-gynecologist at Michigan Medicine, twice has been in her patients' shoes. Both of her pregnancies involved two separate placental disorders.
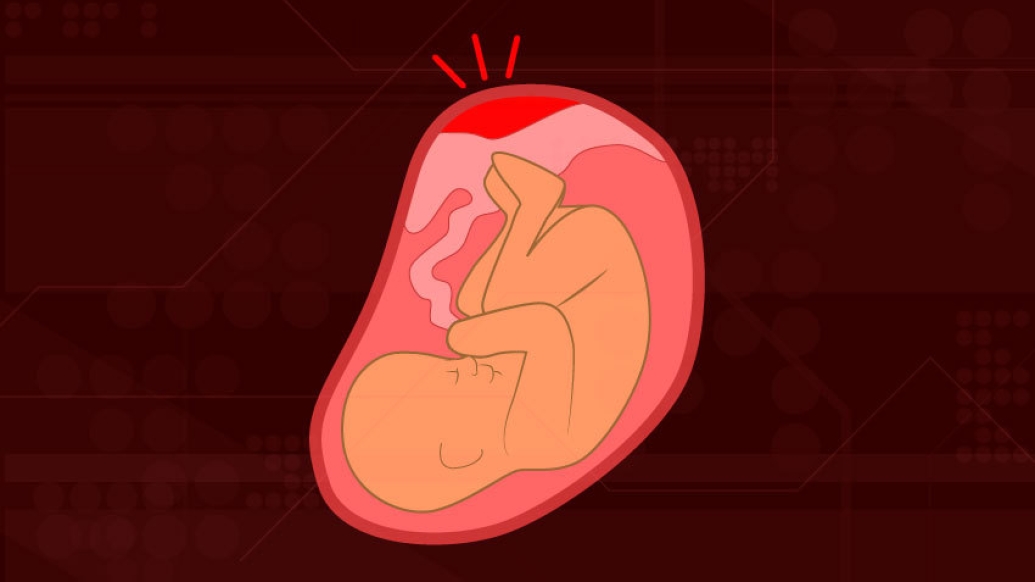
The placenta is a temporary organ that develops in the uterus during pregnancy. It provides the nutrients and oxygen to the baby for development and growth. Because a placenta is created with each pregnancy, it is possible for each pregnancy to have a different outcome.
Even as a trained OB-GYN in good health – she runs and plays basketball regularly – Townsel's high risk pregnancies caught her off guard. Now she wants to share her knowledge. Here are five placental disorders she urges every woman to be aware of before pregnancy.
Placental Insufficiency
Placental insufficiency is the diagnosis that catalyzed Townsel's interest in researching high risk pregnancies. As a first year OB-GYN resident, she was hyper vigilant during her first pregnancy at age 27. Everything appeared to be progressing on schedule until, at 34 weeks, she noticed her baby wasn't growing well and the fluid around her baby was low. Some other moms-to-be may notice the baby isn't moving often. In some cases, the only symptom is the death of the baby.
With this condition, the placenta can't deliver enough oxygen and nutrients to the baby, which may lead to fetal growth restriction and possible issues with the baby's development. The insufficiency occurs because the placenta doesn't attach optimally to the uterus, which impedes the dilation of the arteries and restricts the flow of the important nutrients and oxygen.
To detect placental insufficiency, doctors may order:
-
An ultrasound to look at features of the placenta, calcium deposits or placental thickness, as well as the size of the fetus
-
A fetal nonstress test that monitors the baby's heart rate and contractions
"The diagnosis surprised me," Townsel says. "I had no prior medical conditions. The only thing that slightly increased my risk is I'm a Black woman."
Other potential correlations include having diabetes, high blood pressure, anemia and blood clotting disorders or using blood thinners, drinking alcohol, taking drugs or smoking during pregnancy.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Moms with this condition require frequent visits to a high risk OB-GYN, as well as activity restrictions. Moms need to make sure all possible blood flow is going to the fetus, not to tired or fatigued muscles.
"I had a medical degree and I still wasn't fully aware of the risks that could happen, and that they could occur even if you're young and healthy," says Townsel, who delivered a healthy son at 37 weeks.
Preeclampsia
Preeclampsia, a pregnancy complication that leads to high blood pressure and possible kidney damage, is another placental disorder that Townsel personally experienced.
Its symptoms include excess weight gain in a short period, swelling of the legs, hands and fingers and headaches. Detecting preeclampsia is one of the reasons doctors check blood pressure and measure protein in urine during prenatal care. It can be attributed to autoimmune disorders, genetic factors, diet and blood vessel-related issues. Ironically, preeclampsia also can cause placental insufficiency.
"Often a patient will start to show evidence of placental insufficiency. That can be an indicator of a future complication, such as developing a high blood pressure problem in pregnancy like preeclampsia, hypertension or diabetes," Townsel says.
That was exactly how Townsel's first pregnancy unfolded.
Medical education, health literacy, and advocacy for yourself and others is really important, Townsel says. Women just need to be aware that placental issues can happen. That's how we improve outcomes.Courtney Denise Townsel, M.D.
Her second pregnancy, however, was nearly picture perfect until after delivery. She was 32 and, because of her history, she was taking baby aspirin daily. Global studies have found that daily aspirin improves outcomes and reduces preeclampsia risks by 30%. It helps vessels better attach to the uterus and remain open during the pregnancy, studies indicate.
"My second pregnancy, I took aspirin, the baby grew well, and I went past my due date, but I still developed preeclampsia, but this time it was one week postpartum," she says.
A week after delivery, she was still swollen, never really lost the fluids after giving birth, felt tired and was short of breath. Her blood pressure was high. She ended up hospitalized for 72 hours to receive magnesium to prevent seizures.
The experience made her a more in-tune physician.
"Whenever I start a woman on magnesium, I talk to her from a personal place about how it can make her feel and the concerns of having high blood pressure in pregnancy and how you get through it," says Townsel.
Placenta Previa
Placenta previa occurs when the placenta blocks or partially blocks the cervix, which is the opening to the uterus. This is an issue because a baby passes through the cervix and the birth canal during a vaginal delivery.
Symptoms for this condition include cramps and bleeding typically after 20 weeks. Treatment involves medication, pelvic rest, and activity restrictions, including sex. If the condition can't resolve itself, which happens often, a delivery is typically by Cesarean section.
Researchers aren't certain of the cause of placenta previa but it's often related to women who have previously given birth, had scars on the uterus or are carrying multiple babies. It's found more often in non-white women, those over 35, and patients who smoke or use cocaine.
"While the risks of hemorrhaging and a preterm birth are higher, oftentimes, these pregnancies do just fine if the placenta previa is diagnosed," Townsel says.
Placenta Abruption
A highly dangerous condition for both mom and baby, placenta abruption occurs when the placenta separates prematurely from the uterine wall. This may cut off the baby's supply of oxygen and nutrients, restricting its growth, or prompt a premature or stillbirth delivery.
"This could also lead to heavy bleeding from mom and be life threatening for her, as well," Townsel says. That may usher in transfusions, kidney failure, blood clotting issues or a hysterectomy.
Sometimes it occurs when the mom experiences trauma like a fall, a car accident, or a blow to the abdomen. A rapid loss of amniotic fluid, which cushions the baby in the uterus, could also be the cause.
Other factors that increase the risk are:
-
Hypertension or any high blood pressure-related conditions like preeclampsia
-
Smoking
-
Cocaine use
-
An infection in the uterus
-
Age, especially older than 40
It is not something you can prevent, Townsel says, but you can tamp down the risks by avoiding smoking and drug use. If any trauma to the abdomen occurs, seek a doctor immediately.
Placenta Accreta Spectrum
Sometimes the placenta attaches to the uterus too well. If it expands too far into the uterus, it's called placenta accreta. It may even reach the bladder or wrap around the rectum.
Often this condition goes undetected until after childbirth when the placenta won't detach from the uterine wall. Sometimes part or all of it hangs on. Removing it can lead to severe blood loss after a delivery. Occasionally, a doctor must perform a hysterectomy in such a case.
"Kim Kardashian reportedly had this issue (with her first pregnancy) where her placenta invaded into the uterus and could not be disconnected safely at the time of delivery," Townsel says.
Another related condition is placenta increta, when the placenta invades the uterus' muscles. Placenta percreta happens when the placenta grows through the uterine wall.
The cause is unknown, but risks are higher for those who have had prior surgery on the uterus (previous c-section or other uterine surgery), prior defects in the uterine muscle or in women older than 35. Sometimes it happens for no detectable reason.
"Medical education, health literacy and advocacy for yourself and others is really important," Townsel says. "Women just need to be aware that placental issues can happen. That's how we improve outcomes."

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





