U-M uses patients' DNA and RNA to target and treat cancer
Author |
In children, tumors are more aggressive but are driven by fewer genetic mutations. So you're more likely to pick up the true driver of [tumor] growth. —Rajen Mody

When Melia Miller arrived at the University of Michigan Health System in 2013 to get a second opinion, the 3-year-old girl had already endured chemotherapy, radiation and even the amputation of her left forearm. But none of those treatments halted the soft tissue cancer that was raiding her body.
Then Melia signed on to a new precision medicine program at Michigan that studies and treats pediatric patients who have refractor and rare forms of cancer. An interdisciplinary team combs through patients' DNA and RNA, searching for the exact genetic changes that cause their cancer to grow, then tries to match them with equally specific treatments.
This approach to personalized medicine is an example of the university's ability to not only make basic research discoveries but also use those discoveries to improve clinical care. In the precision medicine program, basic medical research and cutting edge clinical care are tethered together, so advancements in one prompt quick adjustments in the other. By honing this partnership, the U-M has become a leader in the fast-growing field. Results from the first 102 pediatric patients enrolled in the U-M precision medicine program were recently published in the prestigious Journal of the American Medical Association.
Personalized medicine, also called precision medicine, has helped undermine and remake how we think of cancer and how we discuss it. Even within a category — prostate cancer, for example — there are countless variations.
"That's one of the reasons cancer has been so difficult to treat," says Arul Chinnaiyan (M.D., Ph.D. 1999), the S.P. Hicks Endowed Professor of Pathology and of urology at the U-M. "There really isn't one type of cancer — there are hundreds of thousands of cancers."
From Adults to Children
In 2011, Chinnaiyan launched an ambitious cancer sequencing program at U-M with a focus on adult patients whose cancer hadn't responded to standard treatment. Just as they did at the beginning, researchers now take samples of a patient's tumor and healthy tissue, sequence the DNA and RNA of both and compare them. In doing this, they isolate the genetic mutations associated with the disease. They then try to determine which mutations are driving the cancer and to match patients with treatment options that target those mutations.
During an administrative meeting at the U-M Comprehensive Cancer Center in 2012, Chinnaiyan delivered an informal update on this approach. Rajen Mody, M.D. (Fellowship 2000), a pediatric oncologist and U-M associate professor of pediatrics and communicable diseases, was sitting in the back of the room. His patients are all children who have cancer that hasn't responded to standard treatment. As Chinnaiyan described his research, Mody thought: Why aren't we doing this in pediatrics?
Immediately after the presentation, Mody approached Chinnaiyan with a pitch of his own.
"This would actually work better in pediatrics," Mody says now. "Their biology is different. In children, tumors are more aggressive but are driven by fewer genetic mutations. So you're more likely to pick up the true driver of [tumor] growth. And actually, one of the genetic changes — what we call a fusion — is much more common in pediatrics. And Arul's expertise in prostate cancer has been in discovering gene fusions."
Chinnaiyan was eager to collaborate. By the end of the summer, Mody had identified several patients whose families wanted to try this new, personalized approach to cancer treatment. The third pediatric patient the team sequenced was, Mody says, "a complete home run."
Like Melia, the girl had been through multiple rounds of chemotherapy, a bone marrow transplant and more. Genetic sequencing revealed a driver mutation that an existing drug could target. She started taking an oral pill and her cancer went into remission.
"All of a sudden," Mody says, "people started to get really excited."
In some ways, that made Mody's job harder.
"You need those successes to get people's attention. But if it sounds too good to be true … well, it doesn't work in everybody," Mody says. "These are highly desperate families. Even the physicians who are referring these patients are highly desperate."
Mody warns patients and their families that what precision medicine offers is far from a guarantee. Scientists can't always discern which mutation is driving the cancer. When they can, there isn't always a drug available to treat it, or the drug might not work.
Then again, sometimes it does.
A Model for Care
Melia Miller, now 6, lives with her parents and younger brother in a small town in Ohio, two hours from Ann Arbor. She was born prematurely, and with a lesion on her left wrist and forearm. A biopsy performed shortly after her birth was inconclusive. By the time she turned 2, the lesion had grown. Melia was diagnosed with fibrosarcoma, a category of soft tissue cancer, at 26 months of age.
She underwent almost eight months of chemotherapy and two-and-a-half months of radiation in Columbus, Ohio. The treatments left her arm atrophied and hobbled her immune system so much that her parents hired a nanny rather than risk exposure to illness in daycare. Still, the cancer grew. Eventually, Melia's left forearm was amputated.
Three months into a second round of chemotherapy, doctors discovered the cancer had spread to her left lung. Her mother, Lee Ann Miller, then turned to the U-M, contacting Mody in August 2013.
"He wanted to do genomic testing right away," Lee Ann Miller says.
Melia continued to undergo intravenous chemotherapy while U-M researchers analyzed her DNA and RNA.
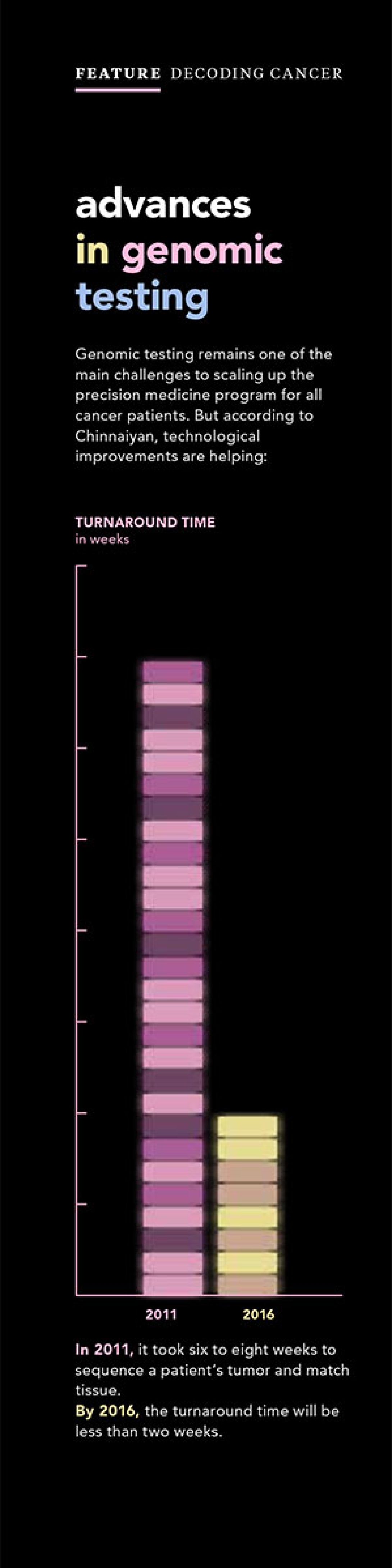
Genomic testing, still a significant undertaking, remains one of the main challenges to scaling up the precision medicine program for all cancer patients. Technological improvements are helping. Chinnaiyan says that when the precision medicine program began in 2011, it took six to eight weeks to sequence a patient's tumor and match tissue. Within the next year, the turnaround time will be less than two weeks.
"That's quite significant when you consider that when the first human genome was sequenced, it took over a decade and over $3 billion. And we're able to turn this around in about a week or two, and cost is generally around $5,000," Chinnaiyan says.
Once the genes are sequenced, the analysis begins.
At 2 p.m. every other Friday, scientists pack into a conference room in the Cancer Center for a precision medicine tumor review board meeting. A wide range of specialists participate: pathologists, oncologists, bioinformatics and bioethicists. The meetings also attract medical residents and laboratory researchers. For two hours, participants talk through eight to 12 cases involving both pediatric and adult patients. For each case, the scientists discuss which mutation could be driving the cancer and what possible treatments exist.
Afterward, the team generates a report for each patient, which includes a rating — one, two or three — of how confident the researchers are that they've isolated the molecular cause of the cancer.
"In some cases, [we find what] has already been linked as a cancer-causing gene through multitudes of studies, cell lines and mouse models … so we can be very confident that it's the driver mutation," Chinnaiyan says. "Then there are cases where there are plausible theories … based on our understanding of how certain types of mutations work."
This is where it becomes critical to have a big pool of data. Useful data include genetic analyses paired with patients' extensive health histories, tested treatments and latest outcomes. With this type of genetic sequencing still in its infancy, limited data means that researchers can't often conclude what's driving the cancer.
More research is needed, and at as many other institutions as possible, Chinnaiyan says. One of his current areas of research aims to improve data sharing to help physicians better interpret the sequencing of a patient's tumor.
When the phrases "personalized medicine" and "precision medicine" were first coined several years ago, many universities were quick to announce plans "that were very ambitious and promised a lot but weren't terribly successful," says Mark Rubin, M.D., director of the Englander Institute for Precision Medicine at Weill Cornell Medical College, who has co-authored research papers with Chinnaiyan.
The U-M, where Rubin was once an associate professor of pathology, has become a leader, he says, in conducting basic research and simultaneously applying those discoveries to clinical care.
"The university refined a lot of what needs to be done, aligning next-generation sequencing so state-of-the-art molecular genomics could be [used] in real-time with clinical care," he says.
Rubin adds that programs like the U-M's precision medicine trial for pediatric cancer "represent a first-in-class type of activity," and that his institution is modeling its clinical trials after those conducted by the U-M.

By the end of 2016, every patient that's seen at our Comprehensive Cancer Center should receive some level of genetic sequencing. —Arul Chinnaiyan
A Really Good Day
By the time Melia Miller's genes had been sequenced, analyzed and discussed by the U-M precision medicine review board, the girl's cancer had leapt from the left lung to the right.
"This was in spite of the 'big gun' chemotherapy," Lee Ann Miller says. "And the cancer just wasn't responding."
The family was devastated. Lee Ann and her husband, Tim, began to mourn the milestones they feared their daughter would never reach: kindergarten, first communion, high school graduation, marriage.
Then Mody called with Melia's precision medicine report. The U-M team felt confident they had identified the genetic mutation driving Melia's cancer. And there was a clinical trial — for an oral biological chemotherapy agent — that targeted it. The drug, crizotinib, is an FDA-approved treatment for adults with certain types of lung cancer.
Grateful for any chance, the Millers gave consent for Melia to start the drug immediately. She stopped the intravenous chemotherapy and instead swallowed two capsules each day. The side effects of chemotherapy disappeared. Her hair grew back, her strength and vitality returned.
Two months later, she went in for a scan.
"Then we got the best news we've ever gotten," Lee Ann Miller says. "We had 50 percent less disease. We were ecstatic."
After three more months on the experimental drug, another scan showed Melia's disease was stable.
"Again, we were ecstatic," says her mother. At Melia's last scan, in June, her left lung was cancer-free.
She is not yet in remission, but her cancer has receded. For the first time, her life resembles that of other children her age. She has a full head of hair, she takes dance lessons and swimming classes and she's enrolled in kindergarten.
Melia's recovery was — and still is — the Miller family's main goal. But it wasn't the only reason they chose to participate in the precision medicine program. Contributing to scientific understanding through research was another priority for the family. Lee Ann Miller now expects to celebrate the milestones she prematurely mourned for Melia.
"If I could prevent anyone else from grieving … I want to do that," Lee Ann Miller says.
Mody says personalized medicine is still a young field of research.
"It's what I would call a completely out-of-left-field discovery," he says.
The U-M team has analyzed about 130 pediatric cases so far. The results of the first 102 patients were recently published in JAMA. About 46 percent of those cases resulted in "actionable genomic findings," Mody says, which means the treating physicians can potentially take clinical actions based on those findings. These actions include using targeted therapy aimed at specific genetic changes, changing patients' diagnoses, and altering how standard chemotherapy or radiation are given or how patients and families are counseled for future cancer risk.
Only 25 percent of the 130 pediatric cases analyzed so far had approved drugs or experimental treatments available through clinical trials that could target the driver mutations identified. Chinnaiyan says that's his biggest frustration — not having more treatment options for patients. Mody adds that in some cases, basic biochemistry studies have to be done before scientists can even begin to develop drugs that target certain mutations. And even when a treatment is under development, paying for a drug can be a challenge for a family.
"Some of these agents can be $15,000 per month," Chinnaiyan says. "Unless you've got compelling evidence that the drug will have an impact, it's very difficult to convince an insurance company to pay."
Even so, the U-M's effort is at the forefront of a field that is growing exponentially and has captured mainstream attention. During his January State of the Union address, President Obama called for more investment in precision medicine. And the topic landed on the cover of a recent issue of Time.
"By the end of 2016, every patient that's seen at our Comprehensive Cancer Center should receive some level of genetic sequencing," Chinnaiyan says.
As a research pathologist, Chinnaiyan doesn't get to meet his patients face-to-face. But he says hearing stories like Melia Miller's are a rewarding — and important — part of his career.
"Our goal is to have the most clinical impact possible," he says. "When we see that this is the mutational driver that we predict and this is the therapy that we suggest and the patient is able to go into remission … that's a really good day at work."





