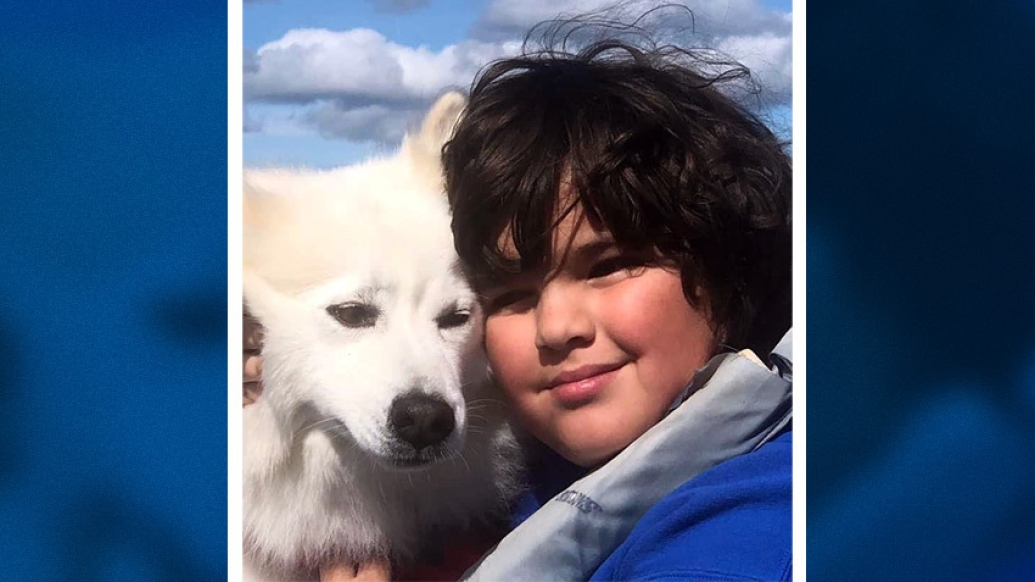
A newborn baby who underwent complex brain procedures grows to be a healthy young boy with a “heart of gold."
5:00 AM
Author |
Lisa Meiners was nearly eight months pregnant when her obstetrician suggested she have a third ultrasound due to concerns with possible scar tissue.
While two ultrasounds are typical during a pregnancy, Lisa wasn't overly concerned when her doctor ordered the third "just to be safe."
As she would discover, the decision was "life-changing."
"A distinct circle was noted in the center of my baby's brain that had not been there on the ultrasound just weeks before. My obstetrician had me drive right over to a nearby radiologist, who immediately identified the condition."
The "possible scar tissue" turned out to be a rare condition known as a vein of Galen malformation, which would require complex endovascular surgical intervention once the baby was born.
A vein of Galen malformation occurs during fetal development and results in abnormal connections between the brain's arteries — the vessels that carry blood to the brain from the heart — and the deep veins that route blood back to the heart. The blood drains into the vein of Galen, located in the base of the brain, and causes an overload of blood flow to the heart. The excess blood can result in congestive heart failure, pulmonary hypertension, hydrocephalus (fluid on the brain) and widespread brain injury.
A vein of Galen malformation begins early in a child's development, likely in the first trimester, says pediatric neurosurgeon Hugh Garton, M.D., of University of Michigan Health C.S. Mott Children's Hospital. If left untreated, the condition generally has a high mortality rate. While open surgical repair was practiced with poor results in the past, advances in neuroendovascular surgical procedures have made survival for many children with this condition possible.
Although 11 years have passed, Lisa and Douglas Meiners still recall in detail their meeting with a team of physicians from the University of Michigan Health and C.S. Mott Children's Hospital. It was during this meeting they learned the serious nature of their unborn child's condition.
Despite their fears, the Meiners had confidence in the U-M Health team, which included pediatric specialists in vascular anomalies, neonatal intensive care, cardiology, neurology, neuroanesthesiology, neurointerventional radiology and neurosurgery.
What to expect
Lisa and her husband, Douglas, listened anxiously as Garton explained in great deal what they could expect in the weeks following their baby's birth.
"Dr. Garton told us exactly what would happen. He explained how the baby would be delivered and taken to the neonatal intensive care unit to be monitored," said Lisa. "We were able to tour the NICU prior to the birth."
Like Podcasts? Add the Michigan Medicine News Break on Spotify, Apple Podcasts or anywhere you listen to podcasts.
The Meiners also met with neurosurgeon Aditya S. Pandey, M.D., who walked them through the endovascular embolization procedure he would perform following the baby's birth.
During this challenging procedure, a small catheter is inserted into an artery in the infant's groin through a small incision. The catheter is guided up to the site of the vein of Galen malformation where a liquid glue-like material or specially designed coils are delivered to the blood vessels to stop the abnormal flow of blood.
"An endovascular embolization reduces the amount of blood flow to the targeted blood vessels. We do the procedure in multiple stages to gradually close off the malformation and ensure the heart becomes stronger," said Pandey. "For a tiny baby, this procedure is technically very challenging. It is a complex procedure that requires a multidisciplinary approach at a facility that offers the most advanced equipment and procedures as well as a highly experienced team."
"Once successfully treated, the blood flow to the child's brain, as opposed to the malformation, becomes more normal and development can proceed as it should. Fluid on the brain, or hydrocephalus, if present, can then sometimes subside on its own."
Lisa was undergoing weekly ultrasounds and echocardiograms to monitor her baby's health. On February 11, 2011, following an echocardiogram, she was advised that labor would need to be induced. That same day, the Meiners family welcomed their son, Rocco, into the world. As expected, the baby was taken immediately to the neonatal intensive care unit, where he was monitored until his surgery on March 4. Rocco remained in the care of the U-M neonatal team for the first seven weeks of his life.
In total, he would have five embolizations – all within 12 months.
"In Rocco's case, without the embolization procedures, he might have died or at the very least would likely have had irreversible injury to the brain," said Pandey. "He was also at risk of heart failure."
Hope and prayers
"When we brought Rocco home after seven-and-a-half weeks in the NICU, there were feeding tubes and many medications," said Lisa. "He couldn't be nursed so we had to put breast milk into his feeding tube." Adding to the stress, Rocco suffered a seizure which required seizure medication and frequent MRIs. He also developed hydrocephalus, which "ultimately dissipated," said Lisa.
The family continued to hope for the best, says Lisa, noting, "The doctors reassured us that our child's brain was still developing. Dr. Pandey told us the brain has a way of creating new pathways that can lead to different and unique talents."
This, she says, could not be more true.
It is a complex procedure that requires a multidisciplinary approach at a quaternary center that offers the most highly advanced equipment and procedures as well as a highly experienced team.Aditya S. Pandey, M.D.
Today, his brain scans show no remaining blood flow through the malformation.
"Dr. Garton showed me the scan and said, 'This is where the spot used to be.' I was taken off guard. I never expected the spot to be completely gone from Rocco's brain." But, she added, "We always had faith Rocco would be fine."
The proud parents describe their son's intense knowledge of the solar system and his exceptional talent as a pianist.
"During a recent school talent show he played 'Rainforest' — which he wrote — and 'Silent Night.' He is also a beautiful artist and loves creating clay sculptures. He imparts emotion in a positive way."
More important, they said, is his "heart of gold."
"We didn't know if Rocco would survive, so seeing him now acting and functioning at a high level is extremely gratifying for the whole team," said Pandey.
Coming full circle
Lisa recalled that day, 11 years ago, when she found out about her baby's condition. It was a cold snowy day as she sat in her car trying to process the news about her unborn baby.
"I don't understand. Nothing bad ever happens to me," she remembered saying. Today, she acknowledges that she has come full circle.
"I look at our life now and, despite Rocco's health as a baby, I again say, nothing bad ever happens to me. This was all meant to be. I wouldn't change a thing."
Live your healthiest life: Get tips from top experts weekly. Subscribe to the Michigan Health blog newsletter
Headlines from the frontlines: The power of scientific discovery harnessed and delivered to your inbox every week. Subscribe to the Michigan Health Lab blog newsletter

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!