Investigators hope to advance the research to larger animals
10:45 AM
Author |
When people think of Alzheimer’s Disease and possible treatment, amyloid — and the accumulation of plaques that invade the cerebral cortex — is often brought up first.
However, scientists are finding that Alzheimer’s is influenced by many factors, including neuroinflammation and disrupted metabolism.
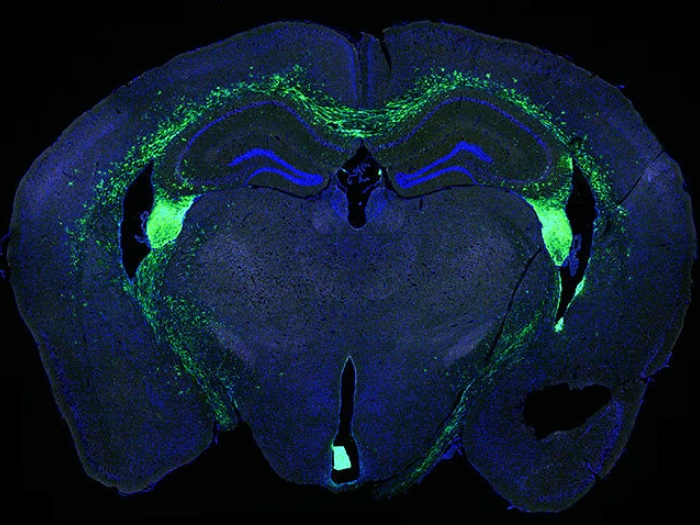
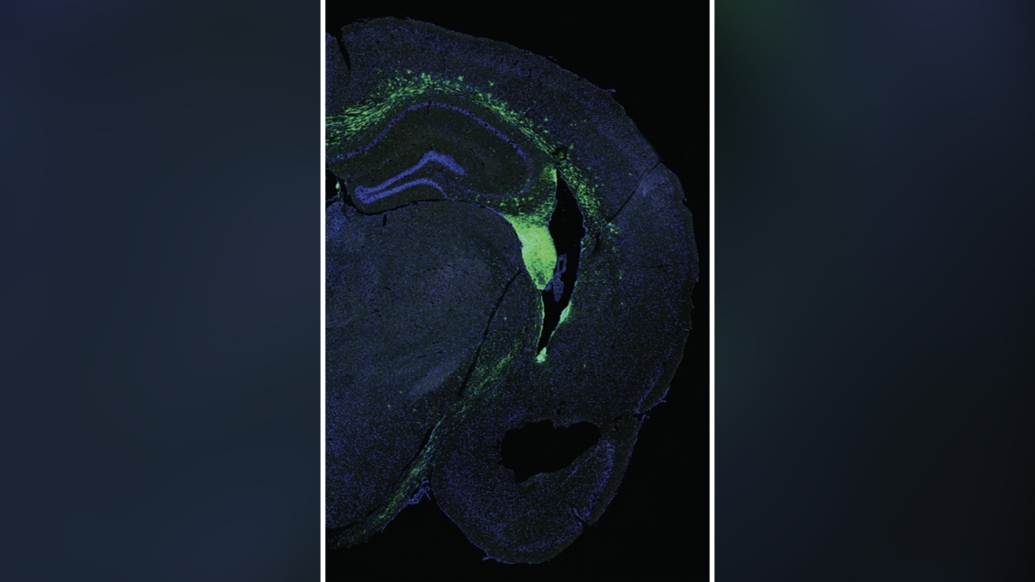
By transplanting human neural stem cells, researchers led by Michigan Medicine improved memory and reduced neuroinflammation in a mouse model of Alzheimer’s Disease, suggesting another avenue for potential treatment.
The results are published in Frontiers in Aging Neuroscience.
“The beneficial effects of transplanting human neural stem cells within the brains of Alzheimer's Disease mice occurred despite amyloid plaque levels remaining unchanged, which lends further evidence that strategies targeting neuroinflammation may be a promising therapeutic strategy, independent of amyloid plaques,” said lead author Kevin Chen, M.D., clinical assistant professor of neurosurgery and neurology at Michigan Medicine.
“Additionally, the treatment was associated with normalized inflammation in the microglia, which are the innate immune cells of the brain that become activated with Alzheimer’s Disease. As the disease progresses, microglia and their inflammatory signaling is thought to contribute to neuron loss.”
A team at Michigan Medicine’s NeuroNetwork for Emerging Therapies transplanted neural stem cells into the memory centers of transgenic mice that expressed mutations associated with familial Alzheimer’s Disease. They had both the test mice and control mice perform a task called the Morris water maze to assess spatial memory and learning eight weeks after transplant.
Investigators found that Alzheimer’s disease mice transplanted with stem cells had their learning curves restored to resemble the control mice with normal learning and memory.
Additional testing through spatial transcriptomics — a method to measure gene expression in areas across the brain— revealed over 1,000 differently expressed genes that were normalized in the memory centers of the Alzheimer’s Disease mice after transplantation.
In analyzing the gene expression changes specifically in microglia, the genetic markers linked to progression of Alzheimer’s Disease were also restored to levels close to control mice. This suggested a reduction in neuroinflammation and disease progression.
Researchers say the improvements reported after stem cell transplantation must be further studied in mice before advancing to larger animals and, eventually, humans.
“Our research is incredibly important and continues to support the promise of stem cell therapies in neurodegenerative diseases,” according to senior author Eva Feldman, M.D., Ph.D., director of the ALS Center of Excellence at U-M and James W. Albers Distinguished University Professor at U-M.
“These preclinical studies are the required first step on the road to stem cell therapies.”
Additional authors: Include Mohamed H. Noureldein, Ph.D., Lisa M. McGinley, Ph.D., John M. Hayes, Diana M. Rigan, Jacquelin F. Kwentus, Shayna N. Mason, Faye E. Mendelson, all of University of Michigan, and Masha G. Savelieff, CRED, of University of North Dakota.
Funding: This research was supported by the National Institutes of Health, The Handleman Emerging Scholar Program, the NeuroNetwork for Emerging Therapies, The Robert E. Nederlander Sr. Program for Alzheimer’s Research, the Sinai Medical Staff Foundation and an Alzheimer's Association grant.
Michigan Research Core: Advanced Genomics Core
Citation: “Human neural stem cells restore spatial memory in a transgenic Alzheimer’s disease mouse model by an immunomodulating mechanism,” Frontiers in Aging Neuroscience. DOI: 10.3389/fnagi.2023.1306004
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of health care news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!