Heart failure with preserved ejection fraction is unique to each individual, requiring a personalized treatment plan and closely monitored care.
7:00 AM
Author |

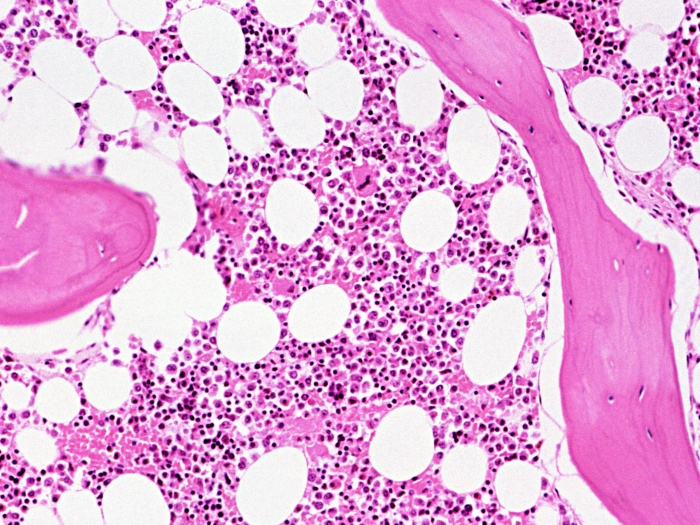
Multiple factors can lead to heart failure with preserved ejection fraction (HFpEF), a condition in which the heart muscle pumps blood normally but still doesn't meet the body's nutrition and oxygen requirements.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Ingeborg Ludeking knows this all too well.
Atrial fibrillation, pulmonary hypertension, an enlarged heart and sleep apnea were among the conditions on a long list of health concerns for the 78-year-old.
Her case isn't unusual. Most patients with HFpEF — pronounced "hef-pef" — also have several other illnesses, says Scott Hummel, M.D., M.S., who directs the University of Michigan Frankel Cardiovascular Center's HFpEF program along with Matthew Konerman, M.D.
"HFpEF develops when one or more chronic medical conditions gradually change the structure and function of the heart and blood vessels," says Hummel. "These changes stiffen the heart and make it more difficult for the heart to fill appropriately, thus limiting the amount of blood pumped with each beat."
Despite Ludeking's many health challenges, the resident of Clinton Township, Michigan, was able to enjoy a relatively active life until four years ago, when she began finding it difficult to breathe.
"I couldn't take more than 10 steps before having to stop to catch my breath," she recalls.
Warning signs
HFpEF symptoms often include:
-
Chest discomfort
-
Decreased exercise tolerance
-
Fatigue
-
Shortness of breath with exertion or while at rest
-
Swelling in the lower extremities
Risk factors
Underlying conditions or factors associated with HFpEF include:
-
Aging
-
Anemia
-
Atrial fibrillation
-
Chronic kidney disease
-
Chronic obstructive pulmonary disease (COPD)
-
Coronary artery disease
-
Diabetes
-
Hypertension (high blood pressure)
-
Inflammatory or autoimmune diseases
-
Obesity
-
Sleep apnea
A heart catheterization in 2015 confirmed Ludeking's HFpEF diagnosis. Her HFpEF risk factors were high, says Hummel, noting that the condition is becoming more widespread as the country's population ages and the associated risk factors become more common.

Treatment for HFpEF
Hummel says treatment for most patients with HFpEF includes controlling blood pressure and reducing excess fluid in the body that can cause swelling or shortness of breath.
SEE ALSO: How to Avoid a Heart Attack While Shoveling Snow
That isn't always enough, however. And reactive measures are often unique to the individual.
"HFpEF is a very complex illness, and there isn't one treatment that works for all patients," Hummel says. "When a patient is diagnosed, we have to sort through the individual aspects of the underlying conditions that contribute to it. We often also use information from diagnostic tests such as echocardiography, heart catheterization, stress testing and cardiac MRI to design the best treatment plan for each patient's particular situation.
"We promote lifestyle modification, including exercise and dietary interventions, which can improve quality of life in HFpEF patients. Each of our patients has a nurse case manager assigned to monitor and support them, and direct pager access to the physician directing his or her care," says Hummel.
A place in her heart
Ludeking was treated with diuretics to reduce the fluid affecting her heart and lungs, beta-blockers to keep her heart rate stable and blood thinners to prevent stroke. Her treatment protocol has proved successful.
"Dr. Hummel and his team have made a big difference in my well-being. I feel better today than I've felt in a long time," says Ludeking, who keeps active by riding a stationary bike, tending to her yard and cleaning her home.
"U-M has a special place in my heart," she says.
Photos by Leisa Thompson

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!