New clinical trial is evaluating a next-generation approach to replacing damaged knee cartilage with healthy cartilage cultivated from a patient’s own cells.
8:34 AM
Author |
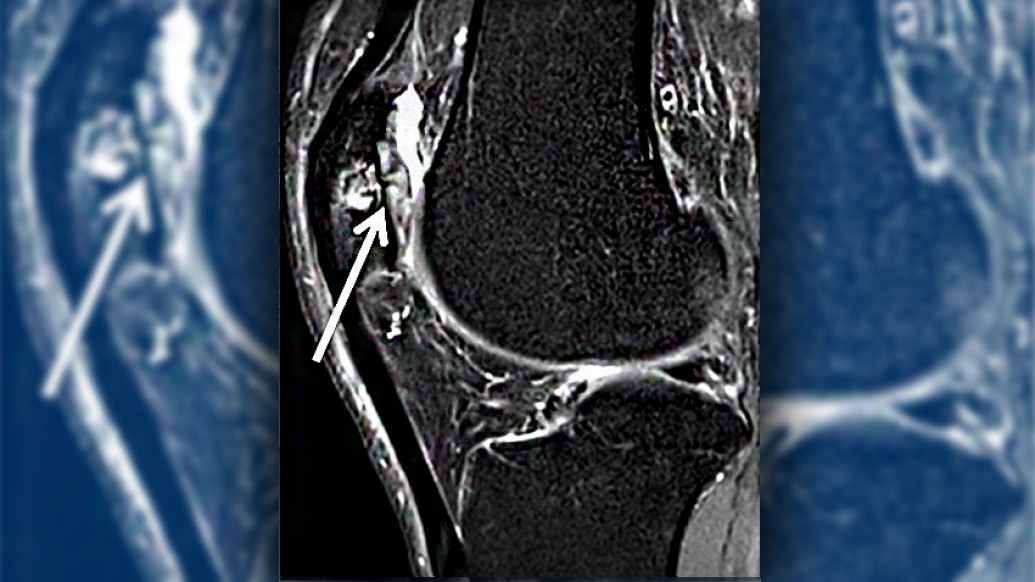
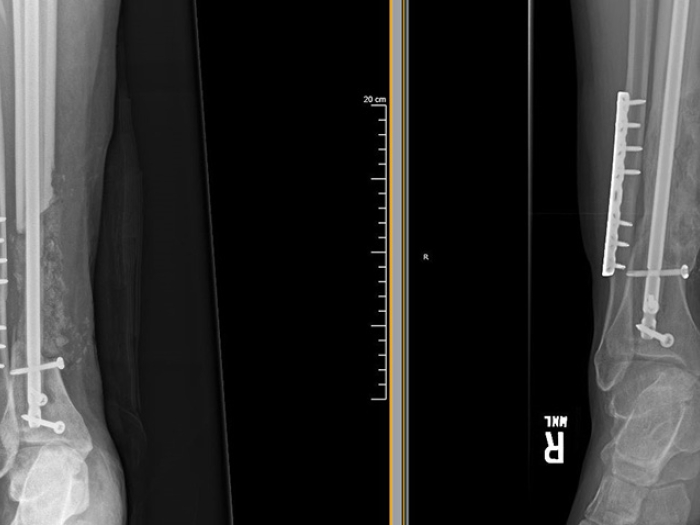
Cartilage, the slippery tissue on the ends of and between bones, provides cushioning and shock absorption. Specifically, in the knee, the articular cartilage at the end of the thigh bone can become damaged from sports or other injuries, or even some illnesses, resulting in progressive pain and loss of mobility.
While a number of surgical procedures have been developed to restore or transplant cartilage, each is limited by the same thing. Compared with other body tissues, cartilage has a poor blood supply, and therefore limited potential to heal itself or to support donor cartilage.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
Now, John A. Grant, Ph.D., M.D., F.R.C.S.C., Dip. Sports Med., an orthopaedic surgeon at Michigan Medicine's MedSport, is leading a clinical trial of a new approach to restoring the viability of damaged knee cartilage. Michigan Medicine is the only site in the state participating in the multi-center randomized study.
About the Trial
The trial is evaluating NOVOCART® 3D, a combination device and procedure that develops "replacement" cartilage from a patient's own cartilage cells (chondrocytes). Two surgeries are involved. First, a biopsy is performed arthroscopically, removing a sample of healthy chondrocytes from the effected knee. In a commercial lab, those cells are expanded and multiplied many times over before being seeded onto a collagen scaffold made to fit the shape and size of the damaged area. In about three weeks, the cells have generated a new piece of cartilage on the scaffold. Then a second surgery is performed to remove the damaged knee cartilage and implant the scaffold with the new cartilage.
The body's own cartilage doesn't heal well, and other options face the same challenge. With this customized implant made from the patient's own cartilage cells, we're hoping for a more durable, long-lasting solution.John A. Grant, Ph.D., M.D., F.R.C.S.C.
NOVOCART® 3D builds on an established technique called autologous chondrocyte implantation. Both procedures replace damaged cartilage with new cartilage cultured in a lab by overlaying the patient's own cells onto a customized structure.
The difference is NOVOCART®3D's new, proprietary structure. The patient's cartilage cells are cultured on to a three-dimensional collagen scaffold covered with a collagen membrane. The scaffold is bioresorbable, meaning it is made of materials that can be absorbed by the body.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
"The body's own cartilage doesn't heal well, and other options such as transplanted donor cartilage and artificial cartilage face the same challenge," says Grant. "With this customized implant made from the patient's own cartilage cells, we're hoping for a more durable, long-lasting solution."
In the randomized trial, patients will be assigned to one of two study arms. One arm will receive NOVOCART®3D. The other will receive a surgical procedure called microfracture. The randomization assigns two thirds of patients to the Novocart 3D group and the other third to the microfracture group. Microfracture involves cleaning up the defected area to expose healthy edges, then drilling small holes in the bone at the base of the defect. Over time, bone marrow cells will rise through the holes to form a clot. When followed by proper rehabilitation, the clotted cells can turn into cartilage.
"Microfracture is the current standard for comparison in cartilage repair as required by the FDA," Grant says. "Patients with small areas of damage who commit to the necessary rehabilitation do quite well for a period of time. Without it, the clots can become stiff, like bone or scar tissue."
An added advantage of the trial is the approval of a companion study arm called a rescue study. Patients randomized into the group receiving microfracture who do not respond well have the option to receive the NOVOCART® 3D implant and continue to be followed as part of the study.
Identifying Good Candidates
"The best candidates for the trial are patients with good overall joint health who suffer from isolated damage to the articular cartilage surface – like a pothole on their knee joint," explains Grant.
Patients with this type of damage often complain of focal pain in one part of the knee, swelling that doesn't go away, or a sensation of the knee 'clicking' in and out of joint.
"The procedure won't address widespread or diffuse knee pain like that caused by arthritis," he said.
To learn more about the NOVOCART®3D trial visit https://umhealthresearch.org/#studies/HUM00119336

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!