Using advanced techniques, Michigan Medicine researchers have created the most complete catalog of cells in the male gonads. The aim: to create sperm in a dish.
7:00 AM
Author |

Nearly 1 in 8 couples in the U.S. face infertility, and about half of those cases can be attributed to semen abnormalities in the male partner.
As the root causes often remain a mystery, new research into the basic biology behind sperm development could one day lead to renewed hope for people wanting to grow their families.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
"Germ cell development is a very complicated process. A lot is still unknown about how mammalian sperm develop and what is driving the differentiation program," says Sue Hammoud, Ph.D., lead author of a new study published in Developmental Cell.
Sperm are germ cells that are continuously generated in the male testes, rendering a man fertile throughout his reproductive life span. Sperm development begins with stem cells called spermatogonia. Like most cells in the human body, spermatogonia are diploid, meaning they have two sets of chromosomes, one from each parent.
Unlike other cells, however, the germline stem cell is the only cell in our body that must go through a process called meiosis, a type of cell division that produces daughter cells with only one set of chromosomes from the original parent cell.
At fertilization, a sperm and an egg fuse to start a new, genetically unique individual.
But deeper insight has eluded researchers.
"The spermatogenesis process is difficult to study because we cannot culture all the required cells in the plastic dish," explains Hammoud, an assistant professor of human genetics, obstetrics and gynecology, and urology at Michigan Medicine.
A detailed search
Much current knowledge of how sperm cells develop comes from examining tissue sections of the testis under a microscope or by analyzing a known population of cells using cell surface markers, which are like ID badges worn by certain types of cells.
MORE FROM THE LAB: Subscribe to our weekly newsletter
Using these labor-intensive methods, researchers defined four major yet varying cell types: spermatogonia (comprised of stem cells and progenitor cells, which are descendants of stem cells), spermatocytes (a diverse pool of meiotic cells), post-meiotic haploid cells known as round spermatids and finally the mature sperm.
Still, the old approaches only analyzed a hodgepodge of commonly found cells, Hammoud notes. Those methods usually missed rarer cell types and key developmental transitions that can help researchers replicate this process in vitro or understand the causes of male infertility.
Only by understanding germ cell and somatic cell interactions can we begin to drive this process efficiently and safely in a dish.Sue Hammoud, Ph.D.
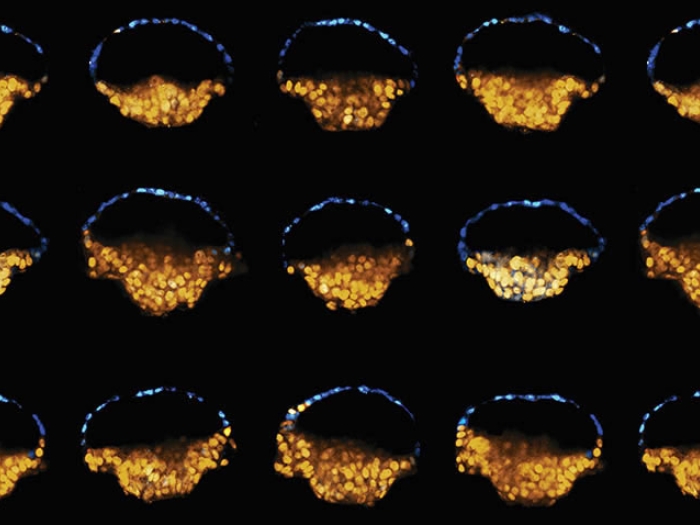
To overcome this challenge, the new study applied a newly developed, advanced technique called single-cell RNA sequencing to separately analyze more than 30,000 cells from mouse testes, measuring the activity of thousands of genes for each cell.
This led to the most complete catalog to date of all testis cells. The team used this data to characterize the sperm cell developmental program and find new cell types and molecular features.
For example, the atlas reveals for the first time that sperm develop in a continuous program, moving seamlessly from one biological state to the next.
"From stem cell to the mature sperm cell, the developmental program is largely continuous, except for a single discrete transition at the entry into meiosis," Hammoud says. "To learn this for the first time is quite remarkable."
Now, researchers can use the knowledge about this program to find the genes that must turn on or off in a precise manner for cells to move through development — a critical step toward finding ways to restore fertility in men who don't produce enough healthy sperm because of inherited or environmental reasons.
Findings inspire future research
While expanding scientists' knowledge of the germ cells, this work also provides the research community new information about somatic cell types and states within the testes that support sperm development.
For example, the work captured known cell types such as Leydig cells, which produce testosterone, and Sertoli cells that act like nurse cells that surround the germ cells, protecting them throughout development and conveying signals from the outside environment.
SEE ALSO: How Stem Cells Grow into Structures That Could Aid Understanding of Infertility
Interestingly, the analysis led to the identification of an unexpected cell population that resembles an embryonic progenitor cell. That has inspired the group's future work to look more closely at these cell types and their potential in the adult testis.
"Only by understanding germ cell and somatic cell interactions can we begin to drive this process efficiently and safely in a dish," Hammoud says.
Hammoud collaborated with Jun Li, Ph.D., professor of human genetics, computational biology and bioinformatics. Their trainees, Christopher Green, Ph.D., and Qianyi Ma, Ph.D., and several graduate students also participated.
These two groups are also among the founding members of the Michigan Center for Single-Cell Genomic Data Analytics, supported by the Michigan Institute for Data Science. This research was supported by National Institutes of Health grants 1R21HD090371-01A1 and 1DP2HD091949-01.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!