A highly complex emergency endovascular procedure was one man’s only hope of survival when others deemed his condition inoperable.
5:00 AM
Author |
As a Vietnam veteran, William Fortner has been through a lot in his lifetime.
A pilot for the military, his history is impressive. And, despite the many missions that might have ended his life, he is here to tell his story, thanks to the expertise of Nicholas Osborne, M.D., and the vascular team at the Michigan Medicine Frankel Cardiovascular Center.
When other surgeons told Fortner he was not a candidate for surgery, a Michigan Medicine team stepped in to perform a complicated emergency endovascular procedure to repair the 77-year-old's thoracoabdominal aortic aneurysm.
The aneurysm had grown to 10 centimeters, "Well beyond when surgery is considered," says Osborne. "This was one of the largest thoracoabdominal aneurysms I had seen." Typically, a thoracoabdominal aneurysm is repaired when it reaches approximately 5.5 to 6 centimeters.
A thoracoabdominal aneurysm is a weakening in the aorta — the major blood vessel that feeds blood to the body. This type of aneurysm extends from the chest to the abdomen and is considered extremely difficult to treat due to its location. But repairing it is critical as a ruptured aneurysm can be life-threatening.
The procedure Fortner would undergo was unlike any that had been done at Michigan Medicine. The highly complex surgery was his only hope of surviving, says Osborne, who headed up the 12-hour emergency operation.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Seeking medical attention
Fortner's health issues had been mounting over the years, with multiple abdominal surgeries and a large abdominal hernia, as well as heart disease. Despite a previous procedure to repair his aneurysm several years ago, his symptoms — including chest pain and shortness of breath — were worsening, an indication the aneurysm was again growing. When his chest pain became unbearable last July, Fortner knew he needed medical attention.
He called 911 and was rushed to a hospital near his home in Cadillac, Michigan, where it was discovered his aneurysm had grown.
"It was a monster and was ready to burst," Fortner says. "I was air lifted to Michigan Medicine and within an hour and a half of getting there, I was in the operating room being prepped for surgery."
Unchartered territory
Osborne was the surgeon on call when Fortner arrived.
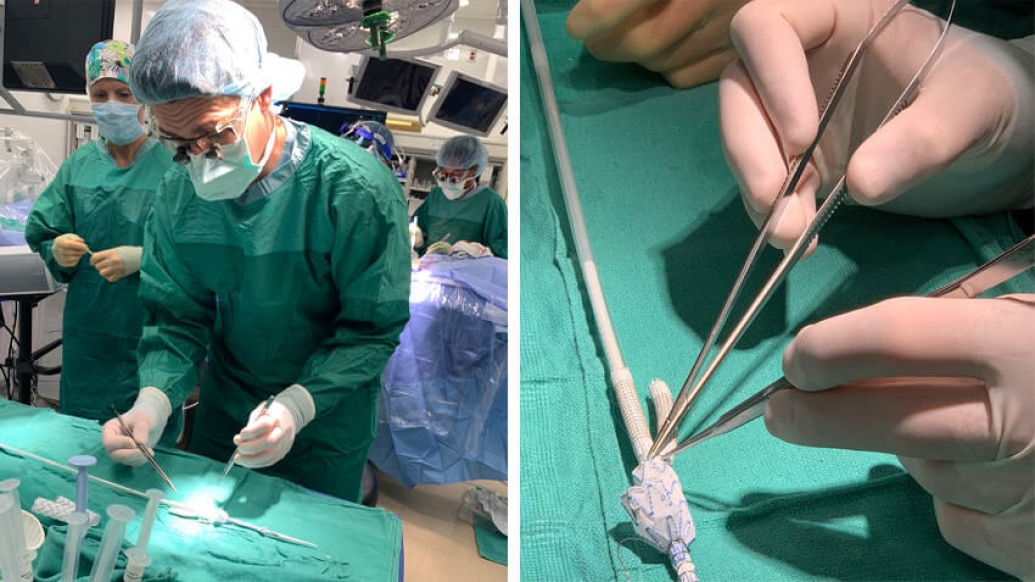
"We saw his condition and discussed with him our novel approach to treatment. This would be his only hope," says Osborne. "We would create a customized repair for him. Only a handful of health systems in the U.S. are doing this kind of thing," he says, referring to it as "a hand-modified, customized thoracoabdominal endograft created in an emergency situation."
The customized repair would require taking a pre-existing woven Dacron tube (graft) covered with stent supports and modifying it by cutting and sewing multiple grafts to fit Fortner's exact anatomy, including his aorta and multiple branches to reach his visceral arteries (supplying blood to his intestines and liver) and his renal arteries (supplying blood to his kidneys).
Fortner was in the operating room while the vascular team was creating the endograft. Typically, an endograft would be customized to a patient's anatomy prior to the actual surgery, says Osborne. "But because it was an emergent situation, we had no choice."
The newly created branched endograft was then inserted through an artery in Fortner's groin and threaded up into his aorta. Next, each of the branches from the graft were extended further with grafts into arteries supplying his stomach and liver, intestines and kidneys.
Although the case was over 12 hours, the majority of the time was spent in planning and creating the customized repair prior to placing it into the body, says Osborne.
"The leap of faith was whether our repair would seal off such a large aneurysm effectively while maintaining flow to his organs."
Osborne says he's one of few surgeons in the country who are custom sewing these endografts for his patients with otherwise inoperable aneurysms.
Like Podcasts? Add the Michigan Medicine News Break on iTunes or anywhere you listen to podcasts.
Seeing beyond the risks
"We had confidence that this would work," Osborne says. "We discussed the risks with the patient — including the possibility that we would not be able to successfully complete the procedure, paralysis due to blocking arteries to the spinal cord, kidney damage, stroke or heart attack.
"He's doing well and is being seen at the Veterans Hospital near his home," says Osborne. "We follow him through the VA system and recent images have revealed his aneurysm is shrinking."
A great sign for Fortner, who has lost 100 pounds since his surgery and is feeling good. He spends his days caring for his new puppy, Ollie, a dachshund who encourages walking — a helpful companion on one man's road to recovery.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!