The mass was putting pressure on her cerebellum and brain stem
5:00 AM
Author |

A Michigan woman is no longer having excruciating headaches after undergoing surgery to remove a large brain tumor that rested above her brainstem and cerebellum.
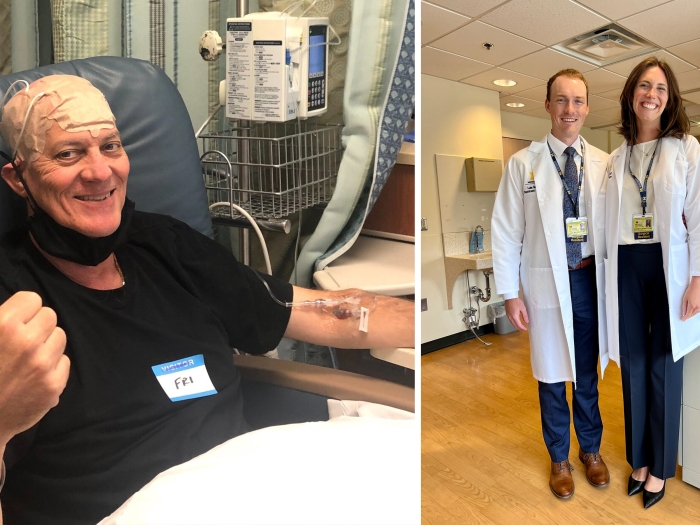
“Everything has changed, and I’m feeling a lot better,” said Paige Gibbons, 21, who lives in Howell, Mich., and had a brain surgery in fall 2023.
“The headaches were limiting my life to where I couldn’t do much. I’m looking forward to driving again and want to go to cosmetology school.”
Headaches and nausea
The symptoms began in high school; Gibbons would get headaches and begin to feel nauseous. She took over the counter pain medication, but the pain and fatigue persisted.
“Migraines run in our family, but Paige’s headaches got so bad that they became paralyzing,” said Rachelle Kedzierski, Paige’s mother.
“I have multiple sclerosis and so does my oldest daughter, and a lot of the symptoms looked similar. But I was floored, sad and scared after we went to the neurologist and got an MRI done.”
The scan showed a large mass — around the size of an orange — inside of Paige Gibbons’ brain.
Pilocytic astrocytoma
They would eventually learn the name: a pilocytic astrocytoma. The slow growing tumor, and the most common brain tumor among children, was large and putting pressure on her cerebellum and brainstem.
It also blocked the flow of cerebral spinal fluid, leading to hydrocephalus. This abnormal buildup of fluid can cause headaches, lethargy and, in the worst cases, coma and death, says Suresh Magge, M.D., pediatric neurosurgeon at University of Michigan Health C.S. Mott Children’s Hospital.
“That’s where the urgency comes, even when the tumor is slow growing like this,” said Magge, who is also surgical director of the U-M Pediatric Brain Tumor Program and a clinical professor of neurosurgery at U-M Medical School.
“After she came to the hospital, Paige was evaluated by the team and taken to surgery the next day. It’s really good that we caught it when we did.”
SEE ALSO: Tumor-destroying soundwaves receive FDA approval for liver treatment in humans
At Mott, Magge explained to Paige and her family that Paige would undergo a posterior fossa craniotomy: he would open the back of her skull and go between the lobes of her cerebellum to find and remove the tumor.
In addition to Magge, the treatment team included pediatric neuro-oncologists, neuroradiologists, pediatric neuroanesthesiologists, nurses, surgical technicians and specialists in intraoperative neuro-monitoring. After surgery, Gibbons was taken care of by the pediatric intensive care team.
“We carefully get around the tumor and separate it from the normal cerebellum and brainstem, with the goal of removing as much of the tumor as we can safely,” Magge said.
Despite needing major brain surgery, Gibbons says she went into the procedure grateful to finally know what was ailing her — and what needed to be done.
“We felt like Dr. Magge was very clear and explained step by step what the process would be like,” Kedzierski said.
“We know that he and the team at U-M have done this many times, and we’re glad we chose there.”
We carefully get around the tumor and separate it from the normal cerebellum and brainstem, with the goal of removing as much of the tumor as we can safely,”
--Suresh Magge, M.D.
Successful surgery
Gibbons’ surgery took place on November 3, 2023. The procedure, Magge says, went extremely well.
“Fortunately, we were able to remove the whole tumor, and Paige did very well after surgery,” he said.
“Her follow-up MRI showed removal of the tumor, and she was able to go home a few days after surgery.”
Gibbons did not require chemotherapy or radiation after her surgery. She’s still dealing with some challenges during her recovery, but the debilitating headaches have disappeared.
“I was really nervous that nothing would drastically change,” Gibbons said.
“There is still a long healing process and some fear because it’s so fresh, but I’m trying to stay calm. We feel like we’re in really good hands with our medical team. I’m excited for what’s ahead.”
Sign up for Health Lab newsletters today. Get medical tips from top experts and learn about new scientific discoveries every week by subscribing to Health Lab’s two newsletters, Health & Wellness and Research & Innovation.
Sign up for the Health Lab Podcast: Add us on Spotify, Apple Podcasts or wherever you get you listen to your favorite shows.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!