A new study examined APS at the cellular level and found that two drugs reduced development of blood clots in mice affected with the condition.
7:50 AM
Author |
For men and women affected with antiphospholipid syndrome (APS), blood thinners are the main treatment option.
"Unfortunately, treatment with blood thinners does not prevent all cases of blood clotting in APS," says Jason Knight, M.D., Ph.D., an assistant professor of rheumatology at Michigan Medicine. APS is an autoimmune condition characterized by blood clots in both genders and pregnancy loss in women.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
"And those blood thinners do very little to impact the neurologic, hematologic and cardiac complications that regularly affect patients with the condition," he adds.
Knight's lab is currently pursuing the idea that anti-inflammatory treatment might provide a more targeted way to treat APS and give patients better control of the condition with fewer side effects.
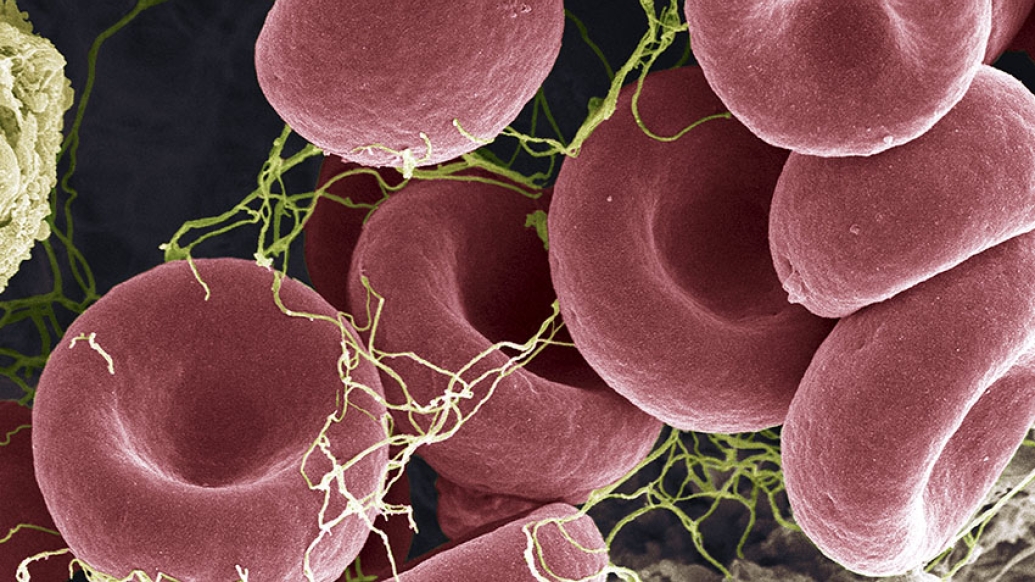
"Specifically, we have been interested in the role that neutrophils, the most abundant white blood cells in circulation within the body, play in APS," Knight says. "We've had prior studies demonstrate that neutrophils release sticky, spider web-like structures called neutrophil extracellular traps, also called NETs, that trigger the blood to clot in patients with APS."
Now, Knight and team are building upon that prior work in a new study, published in Nature Communications, that investigated two drugs and their effects on NETs in mice with APS.
"We explored a new strategy for inhibiting those neutrophils, using experimental drug CGS21680 and an approved drug called dipyridamole," says Knight, senior author of the study.
Testing potential treatments
Using mouse models with APS, the research team first administered CGS21680 and found that it reduced the levels of NETs in their blood.
"The drug works by activating adenosine receptors on the neutrophil surface," says Ramadan Ali, Ph.D., a member of Knight's lab and lead author of the study. "Adenosine is best known for its role in energy metabolism, but also has anti-inflammatory effects when released outside of cells. This appears to be a natural pathway for turning off inflammation."
The research team observed that the drug also dramatically reduced the tendency of the mice to form blood clots in large veins.
The hope is that by continuing to pursue anti-neutrophil therapeutics, we will be treating APS closer to its source and thereby neutralize all aspects of the condition.Jason Knight, M.D., Ph.D.
"Testing this specific drug allowed us to show that activation of adenosine receptors is an effective strategy for preventing NET release in APS, and potentially other contexts as well," Ali says. "We also found that the adenosine-receptor pathway can be exploited to prevent the formation of blood clots."
Because CGS21680 is not approved for use in humans, the research team also decided to test the stroke drug dipyridamole, which has been shown previously to activate adenosine receptors.
"It was very gratifying to see that dipyridamole copied the results of the experimental drug that we began the study with," Ali says. "It reduced both NET release and the tendency of the mice with APS to form clots."
Translating from bench to bedside
While all of the work was preclinical, the research team believes it could be translated to patients with APS.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
"This is what's exciting," Knight says. "We have identified a pathway here that is already influenced by a number of drugs approved for use in humans. Beyond dipyridamole, drugs like apremilast, used in patients with psoriasis and psoriatic arthritis, and methotrexate, used to treat rheumatoid arthritis and certain types of cancer, can also modulate adenosine-receptor signaling."
He adds, "Translating these findings to a clinical trial in patients could therefore be very straightforward."
Based on their findings, the research team plans to move forward with a pilot clinical trial in patients with APS.
"We're very motivated to provide safer, more effective and more individualized treatments for patients with APS we see in our clinic," Knight says. "The hope is that by continuing to pursue anti-neutrophil therapeutics, we will be treating APS closer to its source and thereby neutralize all aspects of the condition."
This study was a multiple-year collaboration across the following authors and their departments at the University of Michigan including: Yogendra Kanthi, M.D. (vascular medicine); David Pinsky, M.D. (cardiology); Paula Bockenstedt, M.D. (hematology); Jose Diaz, M.D. (vascular surgery); and Joan Greve, Ph.D., and Olivia Palmer, Ph.D. (biomedical engineering). Additional authors of the study from Knight's lab include: Alex Gandhi, Srilakshmi Yalavarthi, M.S., Andrew Vreede, M.D., He Meng, M.D., Ph.D., and Shanea Estes, MLI.
The study was funded by NIH-NHLBI (R01HL134846 to Knight) and the lead author (Ali) was supported by NIH-NIAMS through the Michigan Rheumatology training grant (T32AR007080).

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





