Surgeons often remove tonsils and adenoids in children to help treat snoring and mild sleep-disordered breathing. Ongoing research will determine whether surgery or watchful waiting best improves symptoms.
7:00 AM
Author |
When parents peek on their sleeping children to find them snoring away, the scene shouldn't be considered reassuring.
MORE FROM THE LAB: Subscribe to our weekly newsletter
"They might say, 'Sound asleep!' 'That's so cute' or 'They don't snore as bad as my father or husband, so it should be OK,'" says Fauziya Hassan, M.B.B.S., M.S., a pediatric pulmonologist and a sleep medicine physician at the University of Michigan C.S. Mott Children's Hospital.
"It's not perceived to be a problem. The fact is, though, it should be."
Habitual snoring in children, which Hassan cites as occurring three nights a week or more, "is not normal."
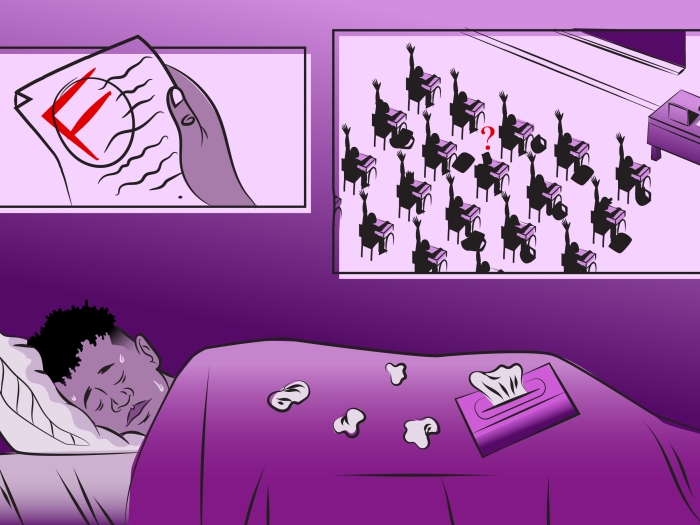
Disrupted sleep because of snoring and the airway obstruction that snoring can represent are associated with disruptive, hyperactive behavior and poor focus in the classroom. In more severe cases, children have an increased risk of hypertension and metabolic disorders.
Which is why many doctors view tonsil and adenoid removal surgery as the logical next step.
Performed more than 500,000 times annually on children in the United States, it's the most common surgery under general anesthesia in that age group. In the majority of cases, this surgery is performed to treat obstructed breathing rather than repeated infections.
However, the impact of surgery on mild sleep-disordered breathing — likely to be present in many, if not most, children who are operated on — is still not clear.
"The data are conflicting right now," says Hassan, who with other U-M colleagues in pediatric otolaryngology and the U-M Sleep Disorders Center is further examining the surgical procedure's effectiveness in snoring children. The research is part of a multicenter clinical trial, sponsored by the National Institutes of Health, known as the Pediatric Adenotonsillectomy Trial for Snoring (PATS).
Hassan pointed to another recent study U-M doctors participated in, the Childhood Adenotonsillectomy Trial (CHAT), which in 2013 found that such surgery was highly effective in improving quality of life and behavior for children with obstructive sleep apnea, a condition characterized by repeated shallow breathing or pauses in breathing during sleep.
But the CHAT study also found that 46 percent of untreated children with obstructive sleep apnea — thought to affect at least a small percentage of children — saw breathing improve naturally, without surgery, during seven months of watchful waiting.
The ongoing PATS trial, led by investigators at Harvard University and the University of Pennsylvania, enrolls patients at U-M and four other centers around the country. Participation in the study can be an opportunity for qualified children ages 3 to 12 who snore but prove not to have moderate or severe obstructive sleep apnea.
LEARN MORE: Find information about participating in the PATS trial
Families of children who participate must be comfortable with random assignment — essentially by the flip of a coin — to have either a prompt adenotonsillectomy or watchful waiting with supportive care. All children in the study receive a sleep study and testing of their thinking and behavior, both at enrollment and again one year later.
Families who participate are helping investigators answer many different questions, but none is more important than the practical one that comes up so often for pediatricians and families whose children snore: If a symptomatic child really does not have prominent sleep apnea, is surgery still helpful?
A lot of times, children are heard snoring softly; it's taken more lightly than in adults. But if they are having issues with frequent nighttime waking up and daytime focus and attention issues, you want to seek help.Fauziya Hassan, M.B.B.S., M.S.
Weighing surgery and alternatives
Determining the presence and severity of a young person's breathing problems requires diligence.
Because most kids and parents don't sleep in the same room, an adult often has little idea of the extent or source of a child's snoring — whether it's temporary from seasonal allergies, for instance, or a long-standing issue. They might not be aware that a problem exists until inattentive, hyperactive behavior during the daytime or a teacher's report indicates otherwise.
A doctor, then, can be a helpful ally.
"If parents think their kids are having behavioral issues and it's not just one-night-a-month snoring, it's worthwhile talking to a pediatrician, a sleep physician or an ear, nose and throat surgeon," Hassan says.
Surgery, she believes, shouldn't come before a thorough examination that could include allergy testing and a sleep study to record and assess breathing during sleep. However, in practice many children are green-lighted for surgery without objective testing for a sleep disorder, Hassan says. The PATS study may more clearly show what role objective data from a sleep study can or should play.
With or without a sleep study, parents and practitioners should work to pinpoint all possible sources of snoring.
Because allergies can cause snoring, finding and removing any possible triggers such as stuffed animals and pets from a child's bedroom — and keeping the space tidy — are plausible steps.
Obesity also can be a factor in whether a person is prone to snoring, so altering diet and exercise could be helpful. Whether the child has a deviated septum might also have an impact.
For those who do need it, tonsil and adenoid removal surgery is common and generally safe, Hassan says, with bleeding and pain after the operation among the minor risks.
"As a clinician, I would say it does work for many children," Hassan says. "A lot of times, children are heard snoring softly; it's taken more lightly than in adults. But if they are having issues with frequent nighttime waking up and daytime focus and attention issues, you want to seek help."
As mentioned above, the PATS trial is currently recruiting participants. Visit UMHealthResearch.org for more information.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!