A review of patient data finds a potential link to costly diabetic eye treatments. It also underscores the need for collaborative care.
1:00 PM
Author |

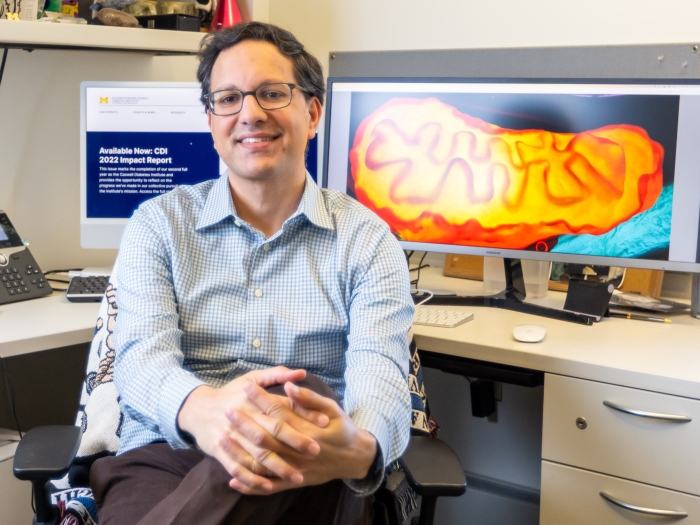
When patients with diabetic retinopathy would see Michigan Medicine ophthalmologist Anjali Shah, M.D., the conversation was often the same.
And it could be frustrating.
"I would tell them what I was taught to tell them: 'You have to get your blood sugar under control,'" says Shah, also an assistant professor of ophthalmology at the University of Michigan.
"A lot of them would reply, 'But my A1c [test] levels are great.'"
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
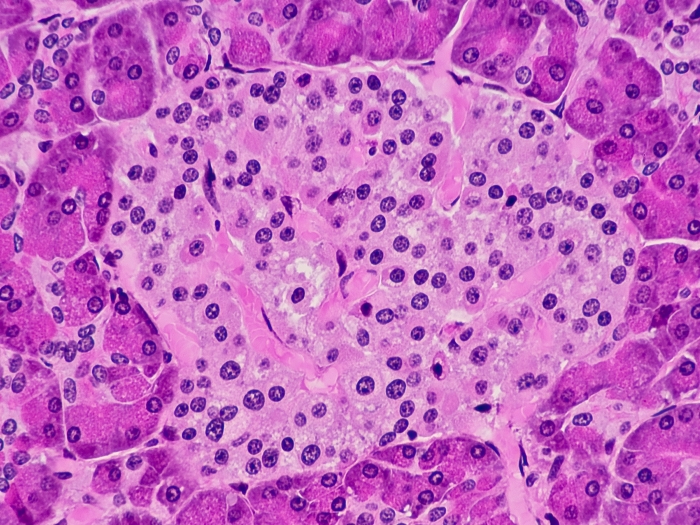
That management wasn't enough to reduce or eliminate the need for anti-vascular endothelial growth factor (anti-VEGF) injections in many patients. The medication is delivered into the eye via syringe to combat diabetic retinopathy — abnormal blood vessel growth and swelling in the retina that can contribute to vision loss.
"I thought, 'There's got to be more to the story,'" Shah says.
Her new research identifies another potential direct link: a patient's blood pressure.
Published in Ophthalmology Retina, the retrospective cohort study examined 2,916 patients treated at U-M's Kellogg Eye Center from June 1, 2016, through 2017.
The review found that systolic blood pressure and a diagnosis of diabetic retinopathy were significantly associated with receiving an anti-VEGF injection, a correlation that eye care professionals could use when counseling patients.
But it's just the start to answering a larger question. "We now need to do a lot more investigating as to what exactly that correlation is," Shah says.
Ophthalmologists ... rarely checked for other risk factors, because they thought it was something a patient's endocrinologist or primary care doctor dealt with.Anjali Shah, M.D.
Finding a connection
The association isn't new.
Eye care providers know that risk factors such as poor glycemic control, duration of diabetes and high blood pressure all contribute to diabetic retinopathy, the leading microvascular complication of diabetes — and the leading cause of blindness in working-age adults.
MORE FROM THE LAB: Subscribe to our weekly newsletter
But they've had little insight into how those factors may predict the frequency and timing of anti-VEGF doses, which can vary widely by individual. (Nor is the need universal; only 21.1 percent of patients in the Ophthalmology Retina study received injections.)
Shah points to prior studies that found a "legacy effect" with glycemic control. Patients who controlled their blood sugar had fewer diabetes-related complications 10 years later, even if their blood sugar had veered off track over time.
That same result, however, did not occur in patients with healthy blood pressure whose numbers then lapsed over a decade — a possible indicator that poorly controlled blood pressure may have an acute impact on need for or frequency of anti-VEGF injections.
There is no defined algorithm for anti-VEGF treatment, however, so patient management can vary widely by physician preferences.
"Our ability to risk-stratify patients and prognosticate for them will change dramatically if studies like this continue to be done," Shah says.

Implications for anti-VEGF treatment
The latest findings, Shah notes, underscore a gap in ophthalmologic care: Eye health providers should do more to help patients with diabetes keep tabs on their overall health.
"There's a division of labor," Shah says. "Ophthalmologists screen and treat eye disease. They rarely checked for other risk factors, because they thought it was something a patient's endocrinologist or primary care doctor dealt with."
SEE ALSO: Dramatic ACA Increase Seen in Insurance for Adults with Diabetes
Helping patients get a better handle on their health during eye appointments could save time and money. Injections, after all, cost $50 to $2,000 apiece — not to mention wages and work time a person may forfeit while receiving treatment.
The extra effort could also help researchers gain more clarity.
"It is very important for ophthalmologists to collect systemic data on patients with diabetes," says Shah, who, as director of the Comprehensive Diabetic Retinopathy Program at Kellogg, has solicited a range of health data from willing patients since 2016.
"That's not routine practice in most clinics and, frankly, is difficult to convince people to do," she says. "But without this data, we will never know how systemic health parameters affect presentation and progression of eye disease."
In the meantime, Shah hopes her work inspires ophthalmologists and clinic aides to take a more vested interest with a few quick questions at each appointment.
It has become a part of her own routine.
"When I see my patients and they're getting frustrated that they need injections every month, I say: 'Make sure you're doing everything you can to manage your blood pressure,'" in addition to glycemic control, medication adherence and other healthful practices, Shah says.
"Diabetes is a systemic disease. It should be addressed with a collaborative team approach."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!