A U-M social worker shares tips to help patients adjust to living with an implantable cardioverter defibrillator.
7:00 AM
Author |
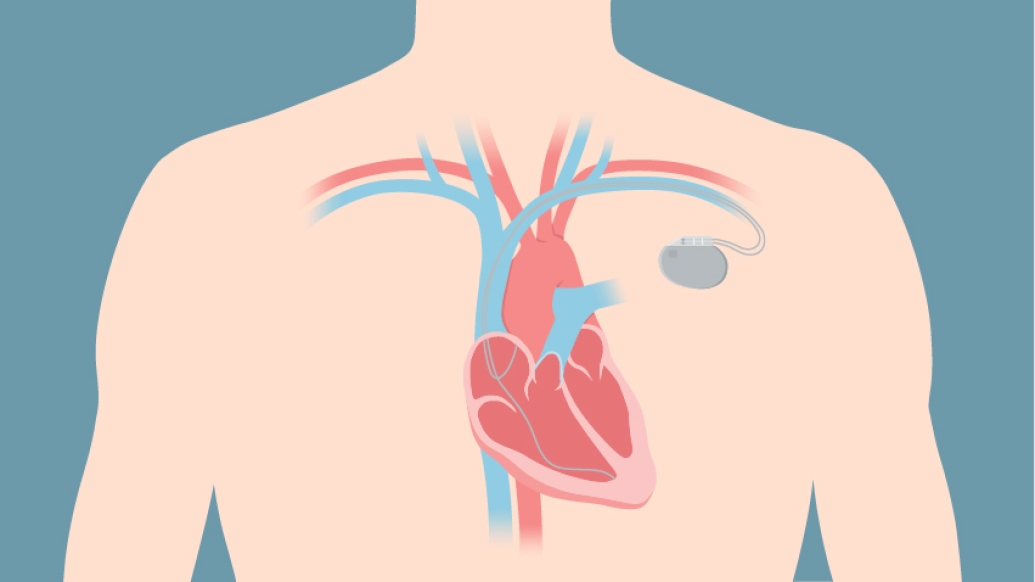
Implantable cardioverter defibrillators are designed to save lives.
They work by delivering either a painless pacing sequence or a jolt of electricity to a person experiencing a life-threatening arrhythmia, or abnormal heart rhythm. But ICDs can also cause anxiety and stress for many patients who have one implanted.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
"Approximately 30 percent of ICD patients have some form of distress related to the device, whether it's anxiety, depression or post-traumatic stress disorder," says Leah Brock, a social worker in the University of Michigan Frankel Cardiovascular Center outpatient clinic.
But, she says, "the way you react to stressful events in your life — whatever form they take — is an indicator of how well you'll adjust to living with an ICD."
Getting shocked is a subjective experience, Brock says.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
"People's feelings about the shock can vary, including their rating of how painful it is," she says. "While a shock is stressful for anyone to experience, the way that a person reacts to and thinks about the shock can affect how much it impacts their future well-being."
Brock's goal is to help ICD patients adapt healthy coping strategies to keep their anxiety from getting in the way of living a full life.
"It's normal to experience some anxiety, but for those who think about their ICD constantly, therapy and medication can be the right solution," she says.
Here, Brock shares five important tips to help patients adjust to living with an ICD:
1. Create a safety plan.
-
Familiarize yourself with your medical clinic's directions on what to do when you're not feeling good and what to do after your ICD has fired.
-
Know whom to notify on your medical team in case you need assistance.
-
Make sure your phone is charged and within arm's reach at all times in case you need to make an emergency call.
-
Let your family or loved ones know where you are, where you plan to be and when to expect you home.
-
When traveling, choose destinations with a hospital nearby so you'll have access to medical care if necessary.
-
Be mindful of how you're feeling and be able to identify symptoms that might lead to your ICD activating. When you feel those symptoms, sit down or pull over to the side of the road if you're driving.
Brock also teaches patients to be aware of the brain's reflexive safety instincts and how they can lead to inaccurate perceptions of safety.
Our anxiety systems are always on the lookout for danger, but they can send false alarms. "Ask yourself, 'Am I safe right now?'" she says. "When patients take a step back to really assess things, they often realize they are fine and it may just be anxiety getting the best of them."
Brock advises patients to become more aware of the unavoidable existence of their anxiety alarm system, including the symptoms triggered by both real and false alarms.
"Your home's smoke alarm will go off if you burn a batch of cookies, but there isn't actually any danger," she says. "Being in the moment helps bring awareness to yourself and your symptoms in order to accurately determine if you are safe or need to seek medical attention."
2. Don't rely on safety crutches.
"Crutches are things that patients incorporate into their lives to give them a sense of control, but in reality they can perpetuate unnecessary anxiety for patients and their loved ones," Brock says.
Common safety crutches include:
-
Constantly checking a personal heart rate monitor
-
Rarely leaving the house
-
Avoiding exercise or activities that may increase heart rate
-
Relying on others for security instead of self-reliance
-
Allowing a worried loved one to tell you what you should or should not do
-
Avoiding things associated with an ICD shock, such as the behavior you were engaged in or the place you were when the shock occurred
3. Avoid "avoidance behavior."
"When patients experience a shock, the brain says, 'That was scary. What can I do to make sure I don't get shocked again?'" Brock says. "Maybe you think it was because you sat in a certain chair, ate a certain food or your morning shower was too hot. Your brain compels you to avoid whatever you feel caused the arrhythmia and led to the shock."
Brock reminds patients that anxiety does not predict the future.
"Thinking or worrying about your device firing does not mean it will happen," she says.
Brock's strategy is to teach patients to gradually expose themselves to what makes them feel unsafe, keeping in mind that the arrhythmia and subsequent shock had little to do with their environment.
"Maybe begin by putting your hand on the chair, then sitting on the chair for a few minutes a day," she says.
Eventually, Brock says, patients realize the chair wasn't responsible for activating their ICD and the anxiety around that stimulus begins to subside.
"We help educate patients to notice and confront their avoidance behavior while aiming to roll with any anxiety it may cause," Brock says.
4. Think of yourself as a survivor, not a victim.
A survivor mentality helps patients accept the reality that their ICD has the ability to save their life.
"Often, patients are distressed about having had no say in getting the device," Brock says. "They may have gone into cardiac arrest, and their emergency treatment included implanting an ICD.
"Instead of being thankful for surviving cardiac arrest, they view themselves as victims."
Brock reminds patients that it takes time to heal emotionally and physically after a major health event.
"Once people realize their strength and resilience, they become more confident and less anxious," she says.
5. Focus on things you can control.
Brock reminds patients about the importance of controlling things they can and letting go of the rest.
She compares this experience to riding in a car: Driving is dangerous, but it's something most of us do without much concern about a potential accident.
"We buckle up, pay attention, use our mirrors and blinkers and go along for the ride because we have places to be, despite the potential danger," Brock says.
Patients can minimize the risk of their ICD firing by taking their medications, practicing wellness activities such as meditation and mindfulness, exercising, being attentive to diet and sleep, reporting symptoms to their medical teams, having their devices and health checked regularly, and following their medical team's directions.
"This doesn't mean they don't need their device — it is still a safety net," Brock says. "Arrhythmias, just like accidents, can be unpredictable.
"I often remind patients that their ICD is there now with a job to do if needed, but it shouldn't hold them back, physically or emotionally," she says. "After an ICD experience, we urge patients to focus on picking up the pieces and getting back to their everyday life as quickly as possible."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!