What turns fungus from friend to foe?
It’s currently impossible to predict what strains of C. albicans will cause infection.
Transcript
Host:
Welcome to the Michigan Medicine News Break, your destination for news and stories about the future of healthcare. Today: What turns fungus from friend to foe?
It’s currently impossible to predict what strains of C. albicans will cause infection.
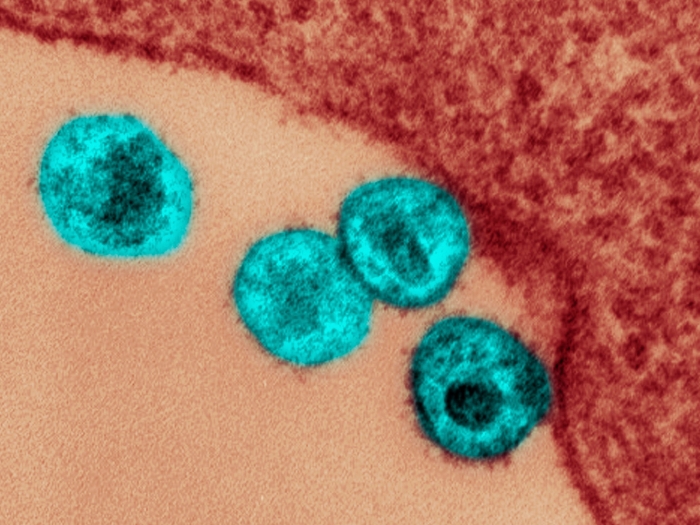
Three out of four women or people assigned female at birth will experience a yeast infection. Many of these infections are caused by an overgrowth of a fungus called Candida albicans. Typically, C. albicans is a quiet resident of a normal microbiome.
Scientists have wondered whether there are differences in the types of yeast that become pathogenic. A study from the lab of Teresa O’Meara, Ph.D. of the U-M Medical School Department of Microbiology and Immunology finds that the colonizing strains are very similar to pathogenic strains.
“Your normal human immune system is very good at controlling fungus, and as a result, we don’t get sick most of the time,” said O’Meara. “It is when we have medical conditions or interventions occur that we can have differential immune responses. It’s not about the fungus, it’s about us.”
People who are immunocompromised, for example, those living with HIV/AIDS, who’ve had transplants, as well as people who are hospitalized or who use catheters, are at increased risk for yeast infections, some of which can be life threatening.
Previous studies have looked at C. albicans samples from people with infections. O’Meara’s team had a unique opportunity to collect samples from 35 healthy undergraduate students.
Using a set of lab assays, they set out to determine how these normal fungal samples grew, whether they were adapted to colonize the mouth versus the gut, and whether they had factors associated with virulence.
“It turns out we could never differentiate between strains in any systematic way,” O’Meara said.
Each strain was able to grow under a wide range of stresses and were able to cause disease in wax worms, used to model yeast infection.
O’Meara admits that while it may sound scary that we are full of fungus that could kill us, fungi also seem to train the immune system against other pathogens or against bloodstream infections from the same pathogen. “We don’t really know all the things it might be doing that are beneficial.”
The findings, suggest O’Meara, should also caution researchers against using any one strain as representative of all.
“There’s lots of diversity in strains but nothing that differentiates a pathogenic strain in the lab. Just as with humans, no one strain or individual encompasses everything possible in a species.”
For more on this story and others like it, visit michiganmedicine.org/health-lab. The Michigan Medicine News Break is a part of the Michigan Medicine Podcast Network and is produced by the Michigan Medicine Department of Communication. You can subscribe to the Michigan Medicine News Break wherever you listen to podcasts.

Listen to more Health Lab podcasts - a part of the Michigan Medicine Podcast Network.
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!