“I’m afraid I never have been much of an ‘I’ll take your word for it’ type of guy,” explains Irwin Futernick. At 66 years old, Irwin finished a journey of finding a solution to his ongoing heart problem. A solution that took him six years and ultimately led him to Michigan Medicine.
And like many with cardiac conditions, it began with a trip to the ER.
“I went into the emergency room and I thought I was having a heart attack,” says Irwin. “It turns out I had something called an atrial flutter, which is when your heart races very, very fast.” To solve this problem, cardiologists at his community hospital performed an ablation to restore the rhythm of his heart. “It was a one-and-done type deal,” he recounts.
While the ablation did help for a time, after five years, he once again found himself in the ER. “I knew something was wrong,” says Irwin, who was now experiencing a new symptom of great difficulty breathing. “This time I had atrial fibrillation and congestive heart failure.” Managing those conditions often requires medications that can slow your heart rate down. As a lifelong swimmer, Irwin’s heart rate was already slow so doctors at his local hospital began considering a pacemaker.
Traditional pacemakers remain the ideal solution for many, but Irwin was resistant. He wanted to avoid the surgery that comes with getting a pacemaker and began to do all he could to bolster his heart health. “I sort of became like a monk,” he says. “In the sense of trying to do only those things that are ‘good’ for you.”
He began exercising regularly and completely changed his eating habits, avoiding salt and fats, reducing his caloric and protein intake, and implementing a plant-based diet, losing 65 pounds in the process. “I had fought hard against the pacemaker,” says Irwin. “It was like my motivator.”
Even with these healthy lifestyle changes, he remained in atrial fibrillation much of the time, which was complicated by his diagnosis of bradycardia (slow heart rate).
A healthy diet and regular exercise can do wonders for cardiovascular and overall health. Unfortunately, however, they have less of an impact on some heart rhythm disorders. Slow heart rates like Irwin’s result from dysfunction of the heart’s natural pacemaker and conduction system (the “wiring” of the heart). Once those systems stop working like they should there is little people can do to reverse the problem.
When Irwin went into his local hospital for a follow-up, his resting heart rate had decreased to a concerningly low 30 beats per minute. Doctors, again, recommended a pacemaker. That’s when he decided it was time to get a second opinion.
His first stop was a clinic that was a level up from his community hospital, which specialized in all things cardiac care. They had the means to do more diagnostic tests and monitored his heart to see exactly what was happening.
The clinic’s tests showed his heart had actually stopped three times over a two-week monitoring period. The doctors there concurred that Irwin needed a pacemaker but, given his active lifestyle, he remained adamant that a traditional pacemaker wasn’t the right fit for him.
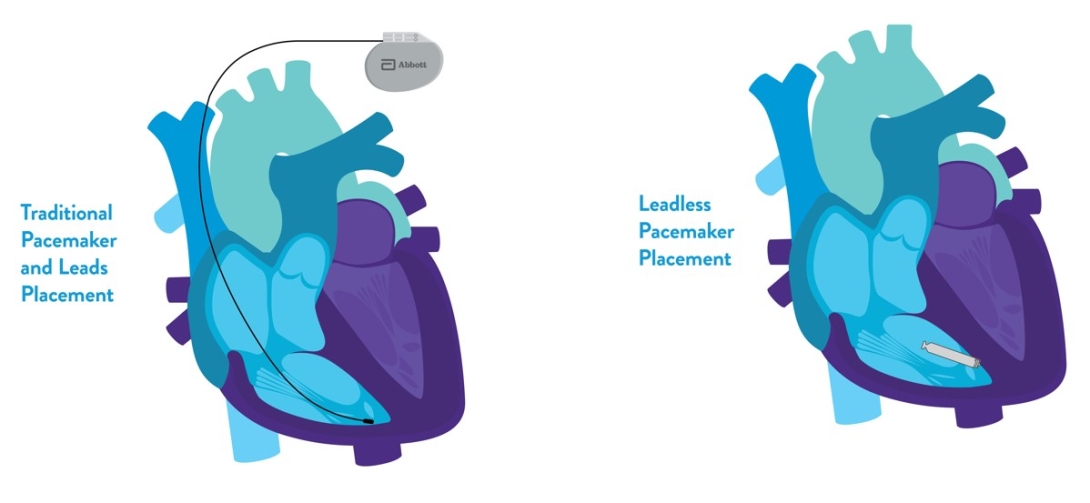
As a former lawyer, Irwin was familiar with doing his own research to discover the facts. “I mean, you talk about recovery time when they do the traditional pacemaker,” says Irwin. “You’ve got these wires running through veins from the generator into places in your heart, and you’re not supposed to lift your arms for weeks.”
So, despite a year of different doctors telling him he needed a pacemaker, which is often exactly what people in his position receive and benefit from, Irwin continued to search for an alternative option that would better adapt to his active lifestyle. That’s how he was put in contact with Ryan Cunnane, M.D., an electrophysiologist at University of Michigan Health Frankel Cardiovascular Center who specializes in cases like Irwin’s, where electric impulse issues influence the heart’s rhythm.
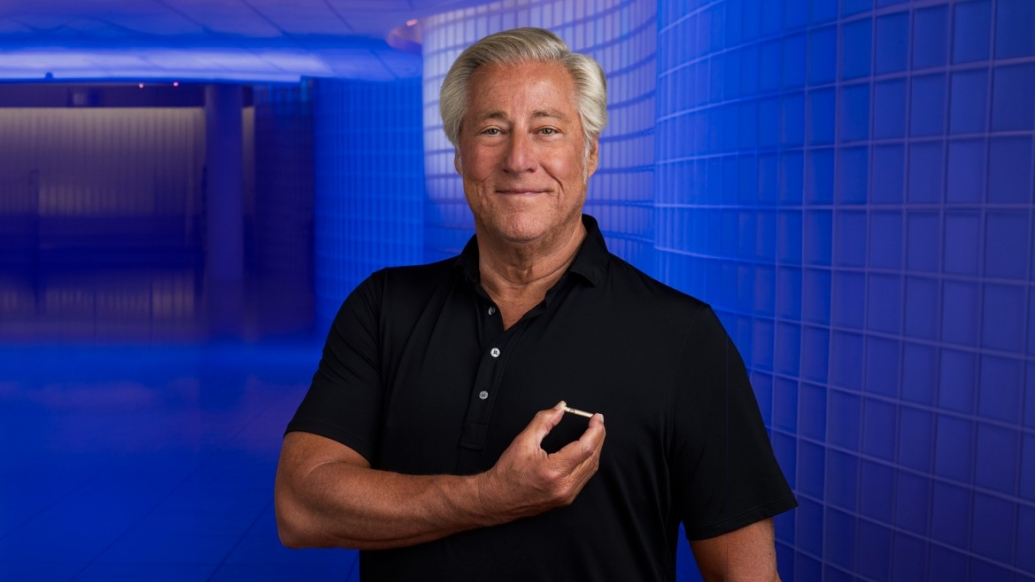
The solution turned out to be a piece of novel technology – a leadless pacemaker small enough to fit on top of a nickel. As the first person in Michigan to perform the insertion of a leadless pacemaker, Dr. Cunnane was the expert Irwin was looking for.
“There are so many advantages to this remarkable device beyond small size,” explains Dr. Cunnane. “Because it has no wires, the weakest link from a traditional pacemaker is eliminated and it has far fewer complications. There’s no surgical incision required for insertion so patients recover much faster and with far lower rates of infection. And perhaps the best part is that since the battery can last around 11 years, patients don’t require follow-up surgery for quite some time,” says Dr. Cunnane.
The leadless pacemaker was exactly what Irwin had been searching for. “Dr. Cunnane was wonderful, very good at explaining things, very good at listening to what I had to say. I appreciated that. He was very patient with us, very generous with his time.”
“My goal before any procedure is to ensure that the patient, and their family, are fully informed and comfortable with the details of what we will be doing, the potential risks, and any alternative options that may be available to them,” says Dr. Cunnane. “I wanted this to be a joint decision between the two of us. Irwin asked all the right questions and, as he learned more about the device, he became more comfortable moving forward with the implant. Open and honest communication is key.”
In August of 2023, comfortable with how the procedure would go and who was performing it, Irwin underwent the successful implantation of this remarkably small pacemaker at Frankel Cardiovascular Center.
“With any medical procedure, a well-informed patient is key to making sure they are comfortable with the rationale behind what will take place and are knowledgeable about what to expect,” says Dr. Cunnane. “Irwin’s case is a great example of how asking questions and exploring all the options can lead to an excellent outcome.”
“I’m glad I kept investigating and searching and discussing,” says Irwin. “I have a sense of freedom with this pacemaker that I wouldn’t have had with the other ones. I was back in the pool swimming a week after the procedure.”

Discover the power of a Michigan Answer through inspiring stories. Find hope and inspiration for your own journey by reading more.