Empowering patients with at-home screenings
We are on the brink of a major shift in gynecological care. The Pap test, developed over a century ago, has been the standard of care for detecting cervical cancer. But it is collected through an invasive and uncomfortable vaginal exam. Michigan Medicine researchers have evaluated several simple at-home tests to detect HPV, a virus that causes cervical cancer. The at-home tests are more accurate than a Pap test and could make screenings more accessible for many people.
When the Pap test was created, researchers found that vaginal cells falling off the cervix could detect cervical cancer. After 100 years of painful cervical scrapings and brushing of the inside of the cervix, we know that this test only has a sensitivity of 50%, which means the test is correct as often as it is wrong, resulting in a high rate of false negatives.
The invasiveness of the Pap test can also deter patients from regular screenings. In collaboration with several diverse community organizations, we recruited more than 120 participants, 30-65 years old, who were not up to date with their cervical cancer screening. They were mailed HPV self-sampling kits at home. After using the kits, they answered questions about their experiences.
Many participants told us that self-sampling provides a comfortable, convenient, and flexible choice without trauma.
“I feel like it was a huge deal to me to be able to do it at home in my own privacy when I was comfortable as opposed to going to the doctor’s office with the doctor and the assistant in the room,” one woman said. “It’s completely uncomfortable for me to do it there, and this made it so much easier for me. I wasn’t anxious about it. I just got it done.”
Self-sampling can be done in one of two ways, either by self-insertion of a device in the vagina or by urine collection. My team is refining a urine collection device that washes the HPV-infected cells already shed from the cervix and vagina. It is as accurate as the vaginal devices and the clinician devices. I’m leading an engineering team to create a system that is meant to be easy to use for patients with disabilities and patients who do not use vaginal products.
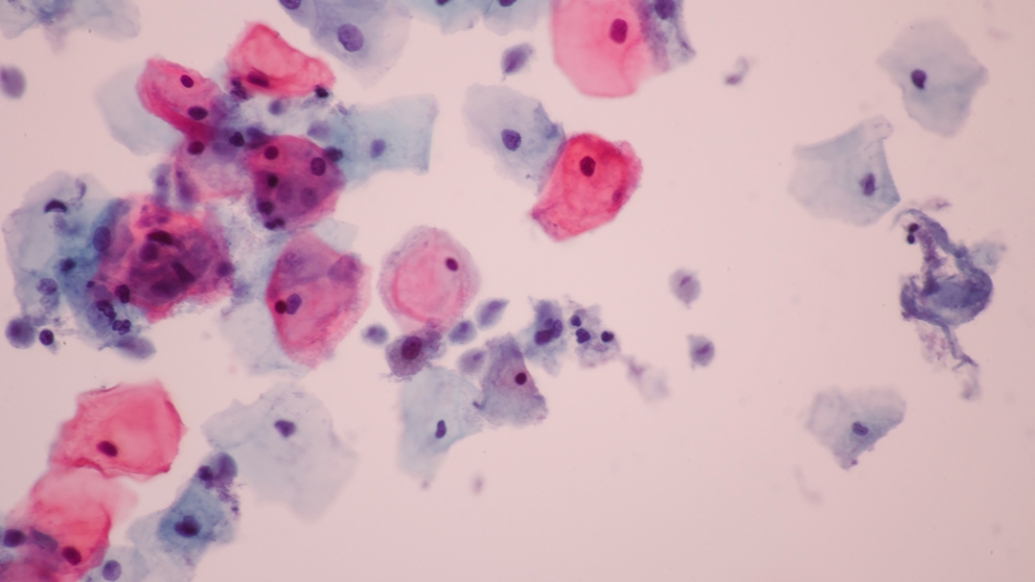
Self-sampling collects cells whose DNA is evaluated for HPV infection, giving us an objective result. But the traditional Pap test subjectively evaluates cell size and shape. HPV testing produces more accurate results and finds existing cancer. And it only requires testing every five years.
This breakthrough is critical for all patients who need cervical cancer screenings, particularly trans men, patients with disabilities, patients who have experienced sexual violence, and others with limited or no access to screening.
“I struggle with PTSD. I was assaulted, so there is always that little bit of anxiety of going in and doing that with someone you are not 100% comfortable with,” another participant told us. “And my doctors never explained to me what they [were] doing. It’s like you come in, you spread your legs, they do their thing, and you leave. So I think this is wonderful. I like the fact that I can do it myself.”
For some patients, both HPV testing and cervical cytology (Pap test) are needed for screening. But for more than 90% of patients, there is now a choice. Through qualitative studies of multiple groups of patients, we found that most preferred self-sampling and said that they would do screenings in the future if they could do it under their control.
“If they said it was time to do another [screening] and I was able to get a kit sent to my house, it would get done immediately,” another woman in the study said. “And I know for a fact that I got a letter from [my health care provider] saying thatI was due another one, and I probably put it off for at least a year.”
This novel screening method can bridge critical gaps in health equity. We are also working with Congress to require the Affordable Care Act to mandate no out-of-pocket costs for follow-up exams and tests after an abnormal cervical cancer screening. I’ve also been tapped by the National Cancer Institute to inform the study design and recruit participants for the study that will be used to gain FDA approval for self-sampling. At-home screenings will help us catch precancers early, avoid poor outcomes, and empower patients in their health care.
Diane M. Harper, M.D., is professor of family medicine, and of obstetrics and gynecology at the Medical School, and professor of women’s and gender studies at U-M. She was elected to the Association of American Physicians in April.





