Bone filler device accelerates bone healing impaired by age or cancer treatment.
11:00 AM
Author |
Within minutes of breaking a bone, the body begins to repair itself.
The immune system sends in cells that act as housekeepers, sweeping out small bone pieces and killing germs. The body forms a soft protective callus to bridge the fracture and blood vessels grow into the area to help the healing.
But when that process is impaired by age, diabetes or radiation treatment for cancer, surgeons at Michigan Medicine are pioneering a device shown to accelerate bone regeneration.
It's well known that radiation kills the angiogenesis process, the phase of blood vessel development critical to bone healing.
"We are developing ways to allow bones to heal when they otherwise wouldn't by looking at introducing blood vessels," says Alexis Donneys, M.D., a surgery researcher at the U-M and lead author of a paper about the strategy published in Nature's partner journal Regenerative Medicine.
The approach is based on delivering a combination of stimulants -- hyaluronic acid and deferoxamine -- into a fracture to grow bone. Small animal testing showed that the therapy dramatically accelerates bone healing after injury.
If you can grow bone in nuclear winter, you can grow bone anywhere.Steven R. Buchman, M.D.
Through a relationship with Kansas University, a unique method was created that, if proven effective in humans, could change outcomes for millions of adults who suffer broken bones each year that don't heal.
U-M's strength in collaborative discovery drove the innovation.
Mark Cohen, M.D., a U-M surgery and pharmacy professor, had been working with Laird Forrest, Ph.D., a professor of pharmacy at KU, on an implantable hyaluronic acid drug delivery system to help cancer drugs reach their target.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily updates on iTunes, Google Play and Stitcher.
U-M colleagues saw an opportunity to combine the technology with their insight in bone healing.
"This modified method for administering hyaluronic acid and deferoxamine with an implantable device eliminates the need for repeat injections," Donneys explains. "This is beneficial for patients since it eliminates pain and discomfort, potential for infection and the time associated with multiple injections."
The device Ferroximend, which earned the U-M's department of surgery's 2018 Michigan Surgical Innovation prize, is capable of delivering the stimulants gradually to the fracture site during the critical period of angiogenesis.
Research suggests a role for deferoxamine in bone repair by inducing bone vessel growth, but its current use is in treating iron overload.
"The data thus far demonstrates that the HA-DFO hyaluronic acid and deferoxamine combination improves upon the use of either compound used singly at the fracture site," Donneys says.
Complications of bone healing
For kids and adults, recovering from a broken bone means weeks or months of recovery. But for the elderly and those who have experienced radiation treatment for cancer, the stakes are higher.
Late film critic Roger Ebert is a notable example. Ebert lost the lower part of his jaw from complications of thyroid and salivary gland cancer treatment.
SEE ALSO How radiation therapy is becoming more personal
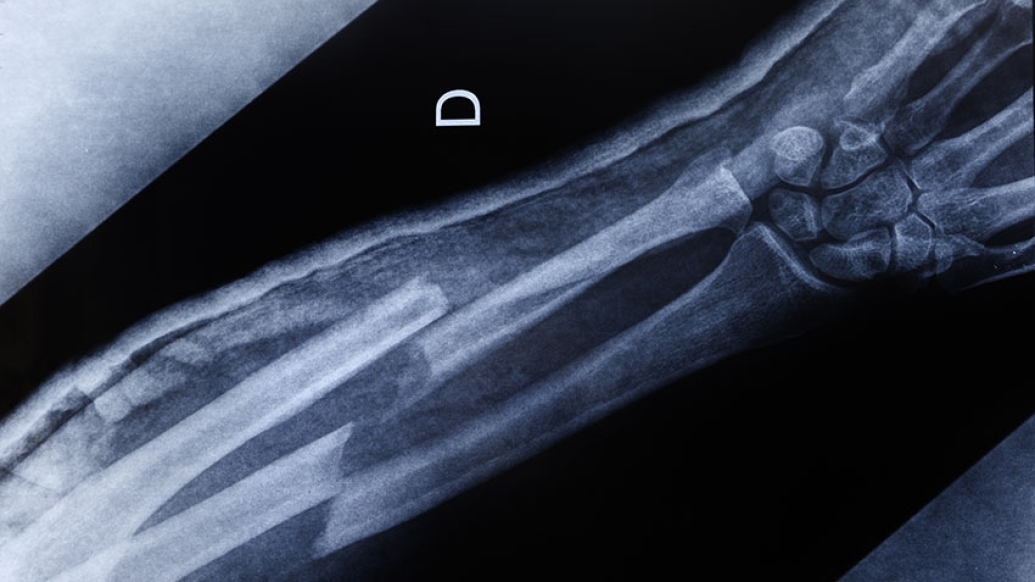
These kinds of large, complex bone wounds often require grafts and multiple surgeries, but just 20% of radiated bone fractures heal, according to the U-M surgeons.
They're hard for doctors and patients alike to contend with.
"We want to do a lot better for patients to help avoid debilitating and disfiguring complications, and improve their quality of life in a way we haven't seen yet," says Donneys.
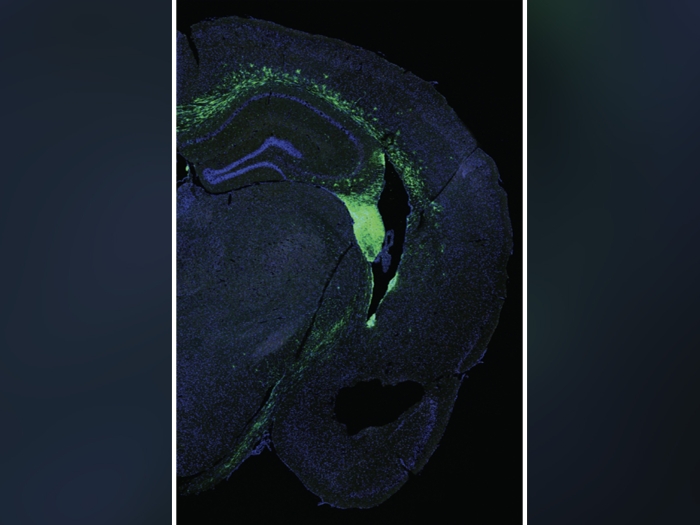
For the study, U-M researchers applied the hyaluronic acid and deferoxamine delivery method to bone fractures in animals that had undergone radiation, one of the most challenging healing processes.
Animals with bone fractures treated with hyaluronic acid and deferoxamine had a 91% bone union rate, which was three times higher than untreated animals, according to the study.
"If you can grow bone in nuclear winter, you can grow bone anywhere," says Steven R. Buchman, M.D., craniofacial plastic surgeon at Michigan Medicine and study co-author.
Looking ahead
As U-M surgeons looked for bright ideas for commercialization, the experimental device had the most promise for improving patient care.
Next the surgery team will use funding, guidance and feedback from its Innovation Prize to focus on pre-clinical studies and regulatory strategies.
One day, the team hopes to see Ferroximend used in operating rooms.
"While most of us were surgically and scientifically skilled, it really felt like we were back in the classroom learning something completely new," Donneys, says of U-M's Surgical Innovation Development Accelerator Course and prize competition.
"The difference was, this time, the lessons we learned could make a big difference in improving surgical practice and patients' lives on a larger scale."
Paper cited: "Implantable hyaluronic acid-deferoxamine conjugate prevents nonunions through stimulation of neovascularization", Regenerative Medicine. DOI: 10.1038/s41536-019-0072-9

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!