Tailoring prenatal care to meet patients’ unique needs, rather than a one-size-fits-all approach, will improve care value and patient experience.
10:10 AM
Author |
During her training, obstetrician-gynecologist Alex Peahl noticed a recurring theme among some of her pregnant patients.
After their 20-week ultrasound to check anatomy, health and gender of the baby, she sometimes wouldn't see them again until weeks before their due date.
"Patients would miss multiple prenatal visits, and the reasons were understandable," says Peahl, M.D., MS.c., an OB-GYN at Michigan Medicine Von Voigtlander Women's Hospital and a national clinician scholar with the University of Michigan's Institute for Healthcare Policy and Innovation.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily updates on iTunes, Google Play and Stitcher.
"Some women had to miss work or needed childcare in order to make appointments. This made me start thinking about how we could right-size prenatal care to more efficiently and effectively serve our patients."
As it turned out, prenatal care delivery recommendations hadn't changed since before World War II. Nor do they match what many patients both want and need,
Peahl's two recent studies in Obstetrics and Gynecology suggest.
And just as Peahl's research on changing prenatal health care models was underway – an unexpected catalyst sped up change: COVID-19. To reduce risk of exposure, clinics began exploring alternative ways to provide care, including virtual visits and consolidated appointments – such as getting the Tdap vaccine and diabetes screening at the same visit instead of separate ones.
"The pandemic has forced us to rethink an outdated system and redesign prenatal care to meet patients' needs," Peahl says.
"We are focused on delivering care around services rather than an arbitrary schedule. In doing so, we've been able to make plans more flexible, patient-centered and give patients a voice in the type of care and services they want in pregnancy."
The pandemic has forced us to rethink an outdated system and redesign prenatal care to meet patients' needs. We are focused on delivering care around services rather than a one-size-fits-all schedule.Alex Peahl, M.D., M.Sc.
Pregnancy care preferences
Based on Peahl's study of 300 postpartum patients, the average patient desires 10 visits during pregnancy compared to the recommended 12 to 14. While almost two thirds of patients preferred fewer visits than currently recommended, 15% wanted more visits.
Most patients in the study also reported comfort with home monitoring skills, including measuring weight, blood pressure and fetal heart tones – which has become more common during the pandemic as more patients stay home to reduce exposure risk.
However, the majority of patients also wanted contact with their care teams between their in-person appointments, such as through phone calls or online messages with a nurse.
MORE FROM THE LAB: Subscribe to our weekly newsletter
"Many women said they wanted prenatal health check-ins without the burden of in-person visits," Peahl says. "They would also like their care to be delivered differently."
Some women wanted more postpartum visits, at least two or three. Others showed interest in alternative care models, such as group sessions where pregnant patients could share experiences with providers and each other at the same time.
And providers are finding that it's not just about medical needs. Through Michigan Medicine's Stay Home, Stay Connected initiative for example, patients also shared interest in seminars with psychiatry, social work or community partners to gain information about coping in pregnancy.
"We usually think of prenatal care as a medical service, but psychosocial support, education and guidance can also improve outcomes," Peahl says.
"Some people will be comfortable with routine services, but we need to take a flexible, holistic approach to serving patients based on their unique needs during pregnancy."
When less is more
The U.S. has the second highest number of recommended prenatal visits than any other high-income country, behind Japan – with women being asked to spend about 40 hours in prenatal appointments, which includes travel and testing time. But an increased number of visits doesn't always correlate with improved care, Peahl says.
"Even though research shows that we can safely care for low risk pregnancies in as few as seven visits, we've traditionally treated all pregnancies as though they are high risk. It has remained as dogma," Peahl says. "But going to the doctor more times isn't necessarily associated with higher quality services or improved outcomes."
In fact, increased visits for low risk pregnancies may even have the opposite desired effect, research suggests. Studies at large hospital systems have shown that more visits may also increase chances of interventions that make induced labor and cesarean delivery more likely.
"Sometimes the more we observe, the more we intervene," Peahl says.
Failing to account for different patient needs may also mean overutilization of some resources and underutilization of others, Peahl says.
"Reducing unnecessary services frees resources and improves access for the most complex patients, who are at the highest risk of maternal morbidity and mortality in pregnancy, delivery, and the postpartum period," she says.
Peahl and colleagues recommend widespread adoption of mechanisms to best identify patients' needs and match them with appropriate services. This includes eliminating a standardized approach to prenatal care and individualizing care.
But the data for high risk pregnant women is more limited, Peahl says. That's why screening for social determinants and underlying health conditions that may increase risk for pregnancy complications will be a crucial part of identifying patients' needs throughout pregnancy.
Virtual care feasibility in pregnancy
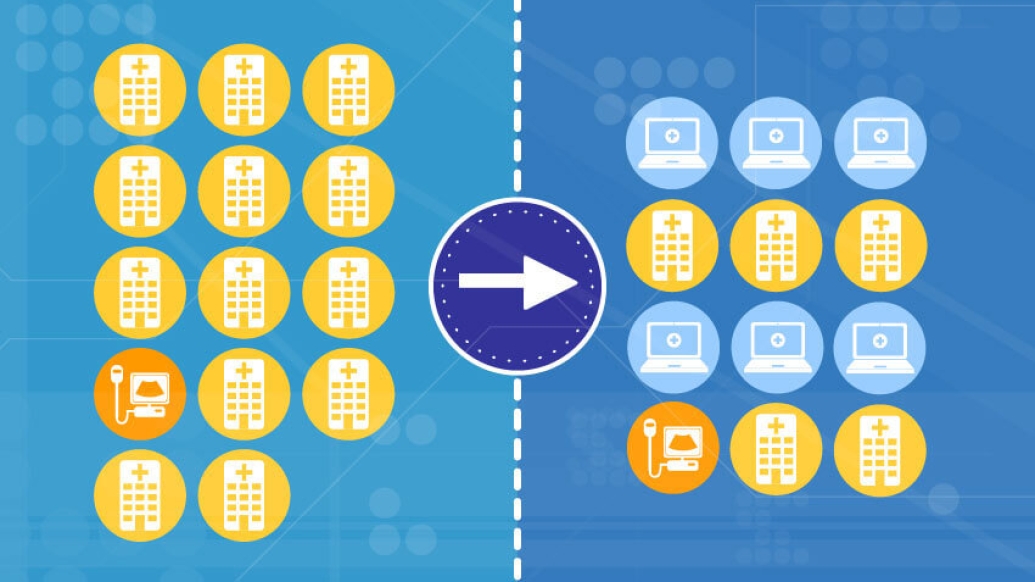
After COVID-19 hit, Peahl led a team that designed a new prenatal care model that alternated telehealth services with in-person visits based on research-backed ways to safely deliver prenatal care for low risk pregnancies.
She says many patients have enjoyed the convenience of remote visits and having access to home monitoring, with the ability to check their own blood pressure and baby's heart rate.
"We found that virtual care is really feasible, and we think in the future it will be an important part of prenatal care," Peahl says. "Many patients find that it's a convenient way to receive prenatal care without disrupting their workday or needing childcare for their other kids."
The next step: policy changes that remove insurance coverage barriers to ending standardized pregnancy care and allowing for more flexible care models.
Further research will also need to examine how changes in services impact low income families and those from demographic populations who may not have the same access to healthcare services or technology that allows for virtual care.
It's important to personalize prenatal care models as well, Peahl says, to fit each patients' clinical, social, and financial needs.
"Tailoring prenatal care to meet patients' medical and support needs, rather than delivering care in a one-size-fits-all fashion, will improve care value and patient experience," Peahl says.
"A customized approach to pregnancy-related services can also optimize costs and outcomes."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





