By trapping tiny numbers of cancer cells from blood , the device can identify whether treatment is working at the four week mark
3:20 PM
Author |
Using a chip to process blood samples, doctors can monitor the amount of cancer cells in a patient’s blood to determine how well a treatment is working by the fourth week, according to a new study published in Cell Reports this week by University of Michigan researchers.
Such data could allow clinicians to adapt cancer treatments to patients’ needs and improve treatment outcomes.
“Currently, there’s typically a wait of weeks to months before we can fully assess the effectiveness of cancer treatment,” said Shruti Jolly, M.D., professor of radiation oncology and associate chair of community practices in the Department of Radiation Oncology at University of Michigan Health Rogel Cancer Center, and a co-corresponding author of the study.
“However, with this chip, we may be able to sidestep prolonged, ineffective therapy and quickly pivot to alternatives, thus saving patients from needless side effects. said Jolly, who is also the chief clinical strategy officer for cancer services at U-M Health.
“This technique has the potential to shift cancer diagnostics, moving from a delayed single assessment to a more continuous surveillance and facilitating the delivery of personalized cancer treatment,”
Liquid biopsies
Today, clinicians use CT scans to see if a tumor shrank or grew, but only large changes in size are easily noticed. Tumor biopsies provide more exact information, but they can’t be done frequently enough to get regular updates.
That’s why many clinicians are turning to liquid biopsies, or tests that look for signs of cancer in the patient’s blood, such as cancer cells that tumors have shed. Blood samples can be collected frequently, but they are only useful if the cells are present in high enough levels for biomedical instruments to detect.
With this chip, we may be able to sidestep prolonged, ineffective therapy and quickly pivot to alternatives, thus saving patients from needless side effects. This technique has the potential to shift cancer diagnostics."
--Shruti Jolly, M.D.
Lung cancer is a particular problem. Other FDA approved tools for detecting cancer cells in blood samples have proven ineffective for monitoring lung cancer treatments—likely because they targeted a single protein on the cells’ surfaces that is less common in lung cancers, the researchers say.
“We were looking for more sensitive markers of cancer that we could use to closely monitor treatments,” said Sunitha Nagrath, a professor of chemical and biomedical engineering and one of the study’s corresponding authors.
“In some cases, only about half of cancer patients respond to the treatments, leaving the rest with poor outcomes,” said Nagrath, who is also co-director of Liquid Biopsy Shared Resources for the Rogel Cancer Center.
“Treatments may also be expensive and cause adverse reactions in some patients, so it’s important for clinicians to know early on whether a treatment is going to be effective—or whether they may be better off with a different treatment.”
Trapping cancer cells
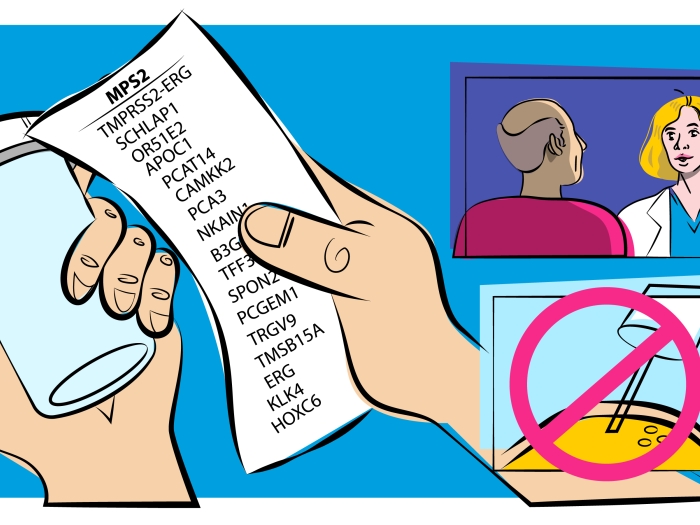
The “GO chip” developed by Nagrath’s team, first demonstrated in 2013, succeeded where others fell short. It traps cancer cells like a piece of flypaper traps flies. But unlike fly paper, the chip only catches its target. Antibodies mounted on microscopically thin sheets of graphene oxide in the chip—which give the device its name—recognize a wide array of cancer specific protein markers found on the surfaces of cancer cells.
As the blood is pushed through channels in the chip, the antibodies trap cells, eventually concentrating enough to work with. With the cells locked in place, the researchers can not only count them but confirm that they are indeed cancerous and determine how the cells’ biochemistry varies between patients and treatment stages.
To test that the GO chip could monitor lung cancer treatments, the researchers used it to collect cancer cells from the blood of 26 patients receiving both chemo- and immunotherapy for stage III lung cancer. The researchers took samples before cancer treatment and after the patients’ first, fourth, tenth, 18th and 30th weeks of treatment.
Targets for future therapies
Their experiment revealed that when the number of cancer cells in a patient’s blood doesn’t decrease by at least 75% by the fourth week of treatment, their cancer is more likely to persist after treatment. The study also showed that cancer cells collected from patients whose cancer did not respond to treatment had activated genes that may have made the cancer resilient. These genes might be good targets for future cancer therapies, but further study is required to test this idea.
The research was funded by the National Institutes of Health. The GO chips were built in the Lurie Nanofabrication Facility.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!