Research finds juvenile myositis and lupus share an inflammatory pathway, but their pathophysiological differences may serve as diagnostic biomarkers in future studies.
10:26 AM
Author |
To date, not much is known about two similar, but different, pediatric rheumatic conditions: juvenile myositis, an autoimmune disease where the immune system attacks its own tissue and causes inflammation in the muscles, and systemic lupus erythematosus, the most common and serious form of lupus where the immune systems attacks its own healthy organs.
The most common form of juvenile myositis is dermatomyositis, which often presents first as scaly, swollen patches or a rash that appears on the skin before muscle weakness begins.
To better understand the differences in these two disease pathophysiologies, Jessica Turnier, M.D., a pediatric rheumatologist at C.S. Mott Children's Hospital and J. Michelle Kahlenberg M.D., Ph.D., a rheumatologist at Michigan Medicine, teamed up with collaborators from Northwestern University Feinberg School of Medicine in an effort to come closer to bringing personalized medicine to the field of pediatric rheumatology.
Kahlenberg and Turnier's study in Arthritis & Rheumatology, the official journal of the American College of Rheumatology, found that juvenile myositis and lupus share a common type I interferon signature, meaning they share a common inflammatory pathway.
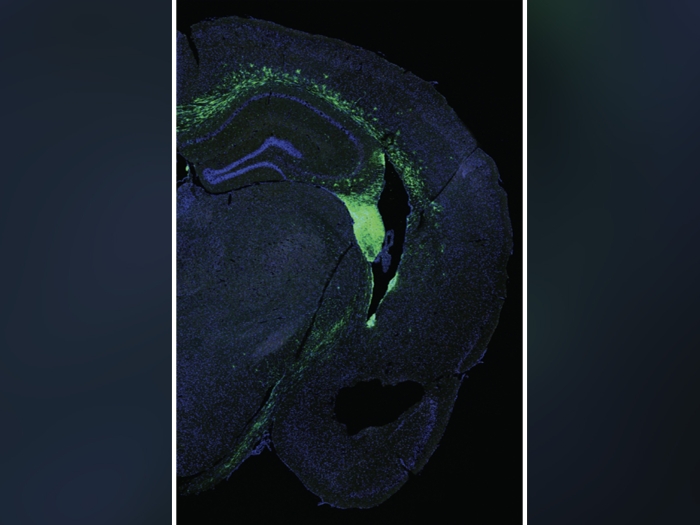
However, after analyzing and identifying differentially expressed genes in skin biopsy samples from 15 patients with juvenile myositis, 5 with lupus and 8 controls, lupus was found to have several more inflammatory pathways turned on compared to juvenile myositis, which only had a predominant type I interferon signature on.
"Both of these multi-system autoimmune conditions can look very similar, but the courses of treatment are quite different and in kids, persistent skin disease can indicate a more aggressive disease," says Kahlenberg. "So it's important to understand what's going on in the skin, what the disease course may look like and how aggressive we should be with immunosuppressive treatments."
According to Turnier, JAK inhibitors, or disease-modifying anti-rheumatic drugs, target lupus and juvenile myositis' common inflammatory pathway, offering potential therapies for the two in three affected children with chronic disease course waiting for clinical care developments.
Notably, an autoantibody found in some of the patients with juvenile myositis, anti-NXP2, was associated with a stronger type I interferon signature, which could be a reason for more serious disease in these kids.
Further investigation into the association of NXP2 autoantibodies and a stronger inflammatory signature may lend insight into the pathophysiological mechanism behind juvenile myositis.
"Although most skin conditions aren't life-threatening, these two diseases greatly impact patients' quality of life," says Turnier. "The child might have to wear clothing that protects them from UV light or else their rashes will get red and inflamed. Or they might have calcinosis, where mineral deposits form under the skin, making it difficult to do things like put on shoes if the deposits are around the ankles."
"Further validation of a juvenile myositis specific skin signature could help clinicians' diagnosis and monitor disease, as well as lead to disease-specific treatment," says Kahlenberg. "We're so thankful for the support from the University of Michigan Advanced Genomics and Research
Histology Core for their equipment and our patients for generously sharing skin samples for our work."
This work was funded by grants to Turnier from the Rheumatology Research Foundation, The Cure JM Foundation and the MICHR. Kahlenberg received support from the National Institute for Arthritis and Musculoskeletal Disease through K24AR076975, a mentoring award, and R01AR071384.
Paper cited: "Comparison of lesional juvenile myositis and lupus skin reveals overlapping yet unique disease pathophysiology," Arthritis & Rheumatology. DOI: 10.1002/art.41615

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!