The first nationwide academic study of physician disciplinary actions and malpractice claims rates shows a lack of standardization across the country.
8:00 AM
Author |

What happens when doctors misbehave? The answer depends greatly on which state they practice in, a new study shows.
In fact, the percentage of doctors who are disciplined or pay a malpractice claim is four times less in some states than other states, the study by a pair of University of Michigan Medical School researchers shows.
And since there probably isn't a fourfold difference in the actual behavior of doctors, the reason for this difference lies in the wide variation between states in their regulations, procedures and resources for punishing doctors who do wrong.
Consumer advocates have noted variation between states' physician discipline rates and standards in the past. But this study, published in BMJ Quality and Safety, is the first nationwide academic evaluation of the topic, and uses statistical techniques to more reliably calculate the actual situation in each state.
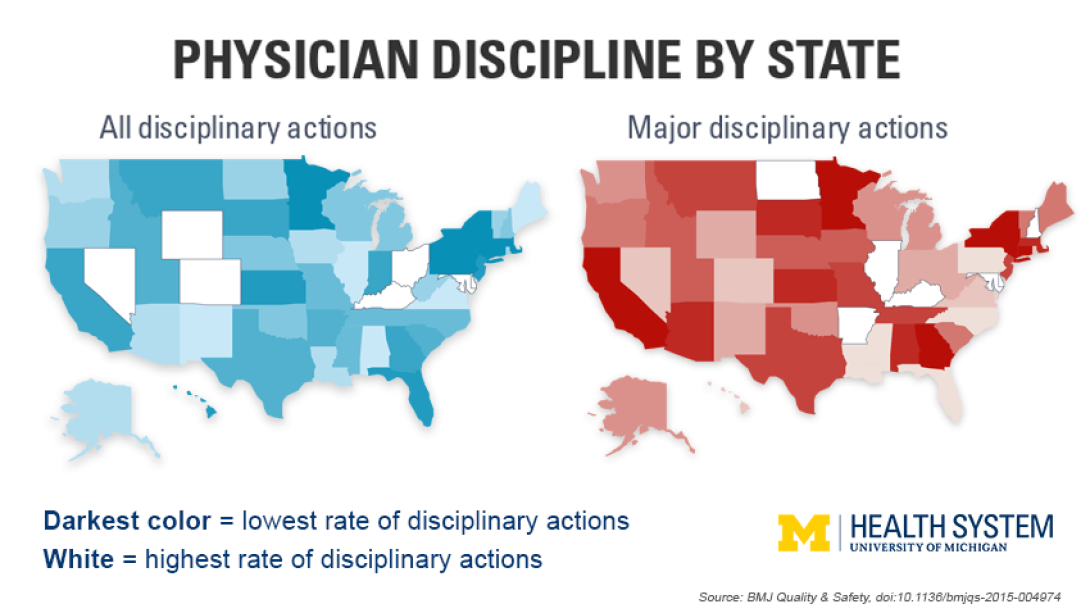
Delaware, Kentucky and Ohio came in with the highest adjusted rates for all disciplinary actions. But it's the states with the lowest rates — such as Massachusetts, New York, Connecticut and Pennsylvania — that should probably look the hardest at their current standards, say the researchers.
"We don't know what the 'right' rate of physician disciplinary action is, but no state should want to be in the extremes," says John A. Harris, M.D., senior author of the new paper. "Patients assume oversight of doctors is well-regulated in all states, that all doctors are held to the same ethical standards and disciplined appropriately when needed. But there's no central governing body, and there's significant variation."
Harris and co-author Elena Byhoff, M.D., are both Robert Wood Johnson Foundation Clinical Scholars at the U-M Medical School and the U-M Institute for Healthcare Policy and Innovation.
This is Harris' latest study of physician misbehavior. The obstetrician-gynecologist has also studied how the rise in female practitioners in his specialty has affected the rate of allegations of sexual misconduct against Ob-Gyn doctors.
We don't know what the 'right' rate of physician disciplinary action is, but no state should want to be in the extremes.John A. Harris, M.D.
National data reveals state variation
The data for the study came from the U.S. Department of Health and Human Services' National Practitioner Data Bank, which covers all 50 states and the District of Columbia. The researchers focused on the most recent data available, for 2010 through 2014.
Since 1986, the NPDB has collected data from each state on actions that state medical boards take against doctors who have been shown to have done something wrong, from substance abuse and sexual misconduct to fraud, negligence and improper prescribing.
The NPDB includes information about punishments including minor fines and required monitoring and major actions such as revoking or suspending a doctor's medical license. It also includes information on payments made by doctors in response to malpractice claims, which the researchers used to create a measure of the malpractice climate in each state. It doesn't include actions taken by individual hospitals that aren't reported to the state medical board.
Hospitals, clinics, state medical boards and insurers routinely access the NPDB when making decisions about which physicians to hire, credential, license or include in their networks. Patients can't access it, and public access to state-level information about individual physicians varies greatly by state, Harris says.
Harris and Byhoff combined all this with information on the number of physicians practicing in the state and calculated a reliability-adjusted yearly state rate of all medical board disciplinary actions per 1,000 physicians.
For the U.S. as a whole, they show that there are 3.75 disciplinary actions each year for every 1,000 physicians practicing — including 1.15 serious disciplinary actions. But the yearly range among states was wide, from 7.93 disciplinary actions of any type per 1,000 physicians in Delaware down to 2.13 per 1,000 in Massachusetts, and from 2.71 major actions per 1,000 physicians in Delaware down to 0.64 in New York.
Medical boards make the difference
The researchers note that in each state, the medical board acts as a self-governing body, with wide discretion on what kind of punishment to dole out for violations of different sorts.
"In one state the punishment for a particular violation could be a fine, while in another state you could lose your license for doing the same thing," says Byhoff. "It has implications for the ability of physicians to move from state to state," if their punishment in one state is not enough to keep a hospital or practice in another state from hiring them.
The researchers hope state regulators and medical boards will heed their findings. Factors such as how easy it is to make a complaint to a state board, how many resources a board has to investigate complaints, the actual makeup of the board, including how many nonphysicians are on it, and the standards for making a judgment and choosing a disciplinary action all play into the variation, they believe.
The U.S. is actually one of few countries that lack a national system for overseeing and punishing physician misbehavior. Australia recently changed over to a central system, after decades with each state or territory having its own medical board. Studying other countries' systems compared with the state-level systems in the U.S. could yield further information about how to address variation and protect the public, Harris notes.
He asks, "Ultimately, don't we want all doctors operating in the same ethical way, and being disciplined appropriately if they fail to do so?"

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!