It’s a chronic skin problem with no cure, but here’s what experts, and especially sufferers, want you to understand about the condition.
5:00 AM
Author |

Psoriasis isn't just about looks, and it's not contagious. And although this rash consisting of red, scaly and patchy spots is one of the more common skin diseases dermatologists see, public misunderstanding persists, says Michigan Medicine dermatologist Frank Wang, M.D.
Wang, who also directs Michigan Medicine's Dermatology Treatment Center, an outpatient clinical program utilizing intensive topical therapies for psoriasis and other inflammatory skin disorders, says it's important to be aware that psoriasis impacts both physical and emotional health.
"It's a condition to be taken seriously," Wang says. "The way patients may be treated by others who are not familiar with psoriasis can really impact their self-esteem and emotional wellbeing."
Here, Wang addresses the five facts more people should know about the condition, which has been a longtime research focus for Michigan Medicine dermatologists.
1. Psoriasis is an inflammatory skin condition diagnosed by a physician.
"It usually manifests as itchy, well-delineated, red, scaly plaques in locations across the body, most often the scalp, elbows and knees," Wang explains.
Patients are typically diagnosed with psoriasis in their 20s or later on in adulthood, usually based on a clinical examination and family history, and sometimes with a skin biopsy to confirm the diagnosis.
SEE ALSO: Why Women Get Autoimmune Diseases Far More Often Than Men
"In addition, we're finding psoriasis can be associated with a variety of other health problems, particularly when it's more extensive, likely because there is inflammation beyond the skin," Wang says. "For instance, patients are at risk for diabetes, high cholesterol, high blood pressure, fatty liver and cardiovascular disease. It also can be associated with arthritis, which often manifests with morning stiffness. Psoriatic arthritis can hinder people's ability to do their normal activities."
2. Psoriasis is not the same as eczema.
Psoriasis is thought to be an autoimmune condition, and it's often confused with the most common form of eczema, atopic dermatitis. Psoriasis lesions typically have sharper borders and thicker scaling than atopic dermatitis, according to Wang.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Patients who have atopic dermatitis will usually start experiencing symptoms in early childhood, Wang says, and it's often associated with allergic conditions, such as asthma, seasonal allergies and food sensitivities. Compared to psoriasis, atopic dermatitis tends to be itchier, less well-defined and present in different parts of the body, like the face and body fold areas of the arms and the legs.
And when people think of psoriasis, Wang says, they're usually referring to chronic plaque psoriasis, which is the most common form of the disease. However, there are other subtypes that cause lesions in different areas of the body than is typical, he explains.

3. Psoriasis is not contagious.
"We know patients can feel distressed or depressed because there's still a lot of social stigma toward psoriasis," Wang says. "Oftentimes, people who don't know what it is may look at lesions of psoriasis and question whether they're infectious – they may ask, 'Am I going to catch it?'"
Wang says psoriasis isn't an infectious disease, and friends, family and strangers shouldn't worry about getting too close to someone who has psoriasis. In fact, genetics play a major role in the likelihood of developing the disease.
4. Research is still ongoing into the causes of psoriasis.
Although research is continuing to advance, there's still more to learn about how and why patients develop psoriasis.
"We're starting to understand the inflammatory pathways involved in psoriasis, and addressing that inflammation is making treatment much more effective nowadays," Wang says.
Genetics play an important part, Wang says, so if someone has a parent with the condition, they are at higher risk for developing it. However, there are likely multiple factors involved that eventually lead to development of psoriasis.
SEE ALSO: Genetic Prediction Model Helps Identify Arthritis Risk in Psoriasis Patients
"In addition to inflammation, environmental factors including medications, trauma to the skin, infection and stress may all play a role in bringing about psoriasis in a person with the correct genetic makeup," Wang says.
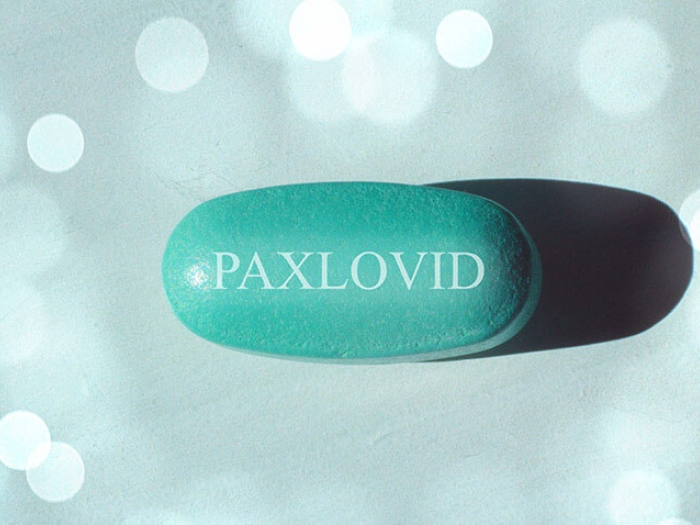
5. Psoriasis treatments have improved greatly in the last decade.
"Today, it's possible to get our patients clear or nearly clear of psoriasis while improving their internal symptoms, including psoriatic arthritis," Wang says.
Treatment options range depending on the extent of the condition, he says, but most work by targeting inflammation caused by an overactive immune system.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily updates on iTunes, Google Play and Stitcher.
Wang's patients with localized psoriasis are more likely to use emollients, topical steroids and perhaps phototherapy (light therapy). Wang says Michigan Medicine is one of only a few specialized centers nationwide that offers an outpatient treatment option, called modified Goeckerman therapy, combining intensive topical treatment and phototherapy for people with very severe psoriasis.
"It's the most effective treatment I have seen in terms of calming psoriasis down within several weeks, although it's time intensive for the patient," Wang says.
He also tends to recommend systemic treatment, like oral and injectable medications, to those whose plaques cover more than 10-30% of their total body surface.
It's important to note that some of these medications have side effects including a greater risk of infection since they target the immune system, Wang says. And newer medications are still expensive, which is an issue that needs to be addressed, he adds.
Finally, because patients with psoriasis have a greater risk of diabetes and cardiovascular disease, Wang says he recommends a team approach in which primary care physicians are actively involved in screening for such conditions.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!