Mapping the changing landscape of gender-affirming care for teens
Rapid state law changes mean 1 in 4 youth now live more than 4 hours from the closest clinic that could provide medications and hormones, and 1 in 4 clinics must stop offering this service.
Transcript
Host:
Welcome to Health Lab, your destination for news and stories about the future of healthcare. Today: Increased Travel Barriers Make it Harder to Access Gender-Affirming Care for Trans Youth. Mapping the changing landscape of gender-affirming care for teens: Rapid state law changes mean 1 in 4 youth now live more than 4 hours from the closest clinic that could provide medications and hormones, and 1 in 4 clinics must stop offering this service.
Many families whose transgender children need gender-affirming care will need to drive much further than before because of laws and other actions passed since 2021 in 20 states, a study shows.
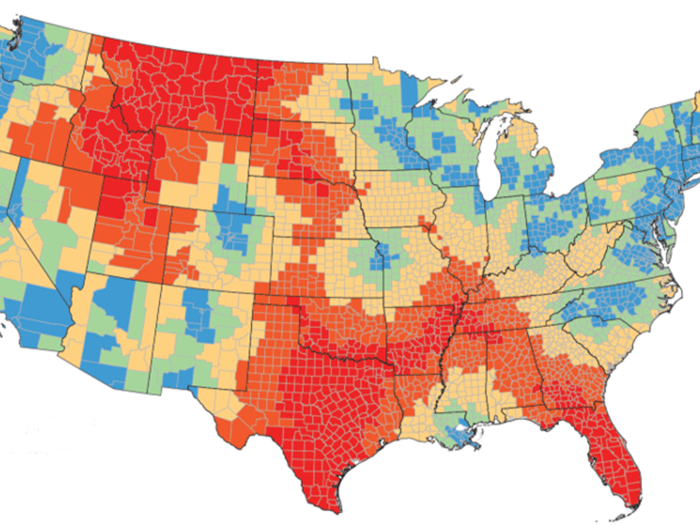
The restrictions mean that 25% of Americans aged 10 to 17 now live more than a day’s drive away, round trip, from a clinic that could provide medications and hormones to support their gender transition. Before the restrictions, less than 2% lived this far from a clinic that could provide such care.
One in four such clinics are in states that now ban this kind of care through legislation, executive action or funding changes, the study also finds. The researchers estimate that 30% of transgender youth – about 89,100 people aged 13 to 17 – live in these states.
Gender-affirming care for teens is supported by several major professional societies, including the American Medical Association, The Endocrine Society and the American Academy of Pediatrics. Inability to access such care has been associated with negative mental health consequences, while access to such care by transgender teens has been associated with reduced depression, anxiety and suicidal thoughts or actions.
The new study, published as a research letter in JAMA by a team from the University of Michigan Medical School, involved online and telephone research to identify 271 clinics that offer medication-based gender-affirming care to people under age 18. It did not include clinics that provide surgical care only. The researchers then mapped travel times to such clinics from the center of every county in the continental United States, before and after restrictions began, and calculated the population of teens who live in each county.
The cutoff for restrictions to be included in the study was May 23 of 2023. Several other states have proposed restrictions under consideration or advancing in state legislatures. Some of the restrictions included in the study are currently paused while court cases are under way, but the study considers what would happen if they are allowed to stand.
In addition to the 25% of teens who would have to travel four hours or more each way to reach a gender-affirming clinic, many more would now have to travel an hour or more.
“Over half of U.S. youth under 18 now, or could soon, face a sizable travel barrier to reaching gender-affirming care,” says Luca Borah, B.A., the U-M medical student who led the analysis along with fellow student Laura Zebib, M.P.H. “It is unknown whether transgender youth and their families will be able to overcome the cost and time barriers associated with out-of-state travel, resulting in delayed treatments or inability to access care.”
Teens in Florida have the biggest jump in drive time to a clinic, with an average added drive of 8.5 hours one way, followed by those in Texas with an added 6.7 hours of driving, on average, to reach the nearest clinic.
For more on this story and others like it, visit michiganmedicine.org/health-lab. Health Lab is a part of the Michigan Medicine Podcast Network, and is produced by the Michigan Medicine Department of Communication. You can subscribe to Health Lab wherever you listen to podcasts.

Listen to more Health Lab podcasts - a part of the Michigan Medicine Podcast Network.