History shows the dangers of relaxing restrictions too soon in a pandemic.
1:35 PM
Author |
Editor's note: Information on the COVID-19 crisis is constantly changing. For the latest numbers and updates, keep checking the CDC's website. For the most up-to-date information from Michigan Medicine, visit the hospital's Coronavirus (COVID-19) webpage.
He helped coin the phrase "flatten the curve." And he's pretty impressed at how well some countries, and American states and cities, have done it in recent weeks.
By keeping as many people at home as possible, they've kept the numbers of serious cases of COVID-19 below or just above what hospitals in most areas can handle, says Howard Markel, M.D., Ph.D. of the University of Michigan Center for the History of Medicine.
And that, without a doubt, has saved lives. It's also bought time for researchers to seek treatments and develop vaccines, and for public health agencies and hospitals to build up the testing and treatment capacity that must be in place before any "return to normal."
But now, Markel worries that some of those places will squander the progress they've made.
SEE ALSO: Flattening the Curve for COVID-19: What Does It Mean and How Can You Help?
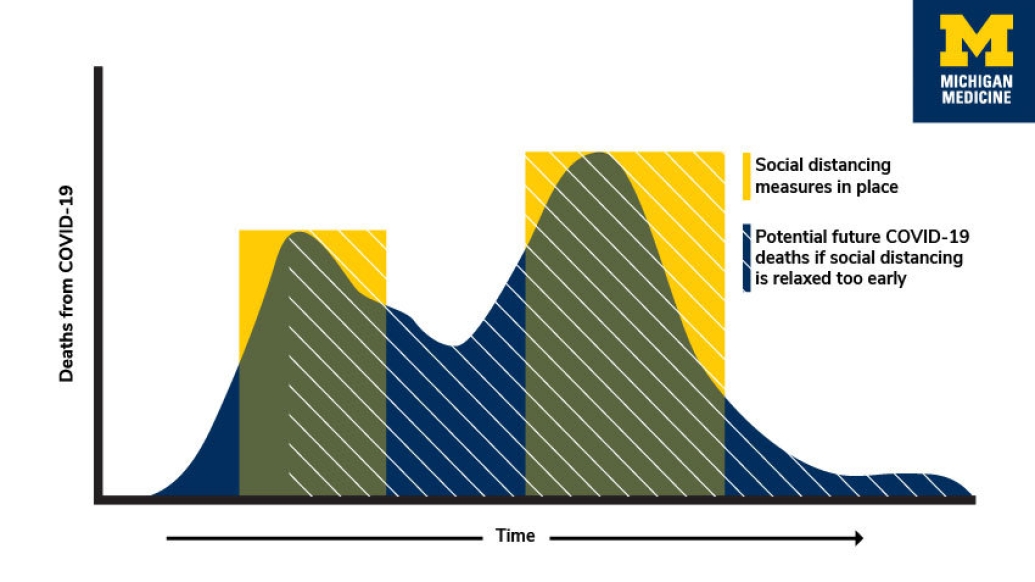
If they take recent signs of "flattening" as a signal to ease up on restrictions, they could end up with something just as bad as, or even worse than, an unflattened curve of COVID-19 cases.
Markel is worried about curves with a double peak.
Easing up on "social distancing" steps too soon, and too quickly, could give the novel coronavirus a chance to race back into broad circulation, he explains. Serious cases, and deaths, could spike again, and waste all the progress that has been made so far.
Lessons from the past
That's exactly what happened in many cities during the flu pandemic of 1918 and 1919, as Markel and his colleagues showed in their detailed study of how non-pharmaceutical measures like school and business closings affected rates of excess deaths in dozens of U.S. cities.
SEE ALSO: Think This Flu Season Is Bad? Flash Back 100 Years
Even though the world of 2020 is far different from that of the World War I period, Markel sees the same thing happening today that happened then, and in other disease outbreaks he's studied.
"In every pandemic, there's a tug of war. On one end, there are the economic and business interests, and on the other end is the public's health," he says. "We know from history that when citizens become restless and protest to their leaders about lifting these sanctions too early, another rise in cases invariably occurs. In some places it was worse than the first peak.
"This creates a situation where you have endured shelter in place sanctions and crippled the economy for nothing," says Markel, a professor of medicine, history and public health at U-M and member of the Institute for Healthcare Policy and Innovation.
Echoes in economic arguments
One hundred years ago, U-M Medical School dean Victor Vaughan described "bodies stacked like cord wood" during his trip to Boston to address the flu pandemic with the Army Medical Corps.
Images emerging in recent weeks from New York City and Detroit, of body bags in hospitals lining hallways and stacked in refrigerated trucks, evoke a modern version of what Vaughan saw.
But at the same time, Markel hears the calls, and even protests, for Michigan and other states to reopen now that the numbers of cases and deaths appear to be starting to level off, or even falling.
Those making an economic case for reopening businesses, schools and public places right now are also echoing the sentiments seen in the popular media of 1918 and 1919, Markel notes.
We know from history that when citizens become restless and protest to their leaders about lifting these sanctions too early, another rise in cases invariably occurs. In some places it was worse than the first peak.Howard Markel, M.D., Ph.D.
But he does see that some in the business community today are looking at another important lesson of the hundred-year-old pandemic: Those cities that kept their citizens out of public spaces longer fared better economically in the long run.
Differences between then and now
The biggest difference between dealing with a pandemic in 1918 and dealing with one now? Without a doubt, it's the power of modern medical science to make much more rapid progress than the World War I generation could ever have imagined. That speed, though, may also make people more impatient for answers.
MORE FROM THE LAB: Subscribe to our weekly newsletter
Another difference: the power of modern medicine to keep many people alive with cancer, heart disease, lung disease and other conditions who would surely have already been dead if they'd developed those conditions in 1918. But now, they're facing the highest risk of dying if they catch the virus.
Markel also points to another difference made possible by technology: the fact that many people – but certainly not all – can continue to do some of their work from home. And that government agencies can get information about relief measures for individuals and businesses out rapidly and without requiring in-person contact.
But for all these reasons, enduring the current hardship, and working to ensure that those most affected get support, is that much more important.
"If we don't listen to the experts in infectious disease, epidemiology and pandemic preparedness, and follow their lead, we will all be contributing to the spread of this virus," says Markel. "As a historical epidemiologist, I really don't want to see my research play out before my eyes."
Returning to "normal"
So when will it be safe to loosen restrictions? We will need to be much further down the far side of the curve that we've just spent so much time flattening, he says.
The epidemic curve of known cases in every city, state and nation has a 'turning point', or what Markel calls an "inflection point", on the way up from where the virus circulated among so many that it's no longer possible to contain its spread.
And on the other side of the peak, there will eventually be a de-inflection point, when cases stop piling up and the epidemic quiets itself down.
It's not possible to exactly pinpoint the downward inflection point, especially in the absence of broad testing, he cautions.
But the ability to test everyone with symptoms, and then to perform "contact tracing" by identifying and monitoring everyone they came in contact with just before they got sick, will be vital to the process of returning to normal. So will a cautious approach for people with underlying conditions and other factors that put them at higher risk. And of course, development of effective treatments and vaccines.
"If you ask me, I will always err on the side of the public's health," he says. "And I think that's true for any of us who are on or near the front lines of this pandemic, and seeing the horrifying carnage it's causing because we don't yet have an effective treatment or vaccine. We need to stay the course, prevent more deaths and buy more time. We are better off safe than sorry."
Like Podcasts? Add the Michigan Medicine News Break to your Alexa-enabled device or subscribe for updates on iTunes, Google Play and Stitcher.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





